Weekend update

Happy Halloween!
The U.S. House of Representatives and the Senate will be engaged in floor voting and Committee business this coming week. The Hill brings us up to date on Democrat Congressional leadership negotiations over the social spending budget reconciliation bill. Bloomberg adds
While the $500 billion infrastructure bill has already passed the Senate, the larger economic package will have to return there for another vote. Some Democratic Senators are signaling they may seek changes to what is passed in the House, possibly adding further delays.
From the Open Season front, the ACA marketplace open season resumes tomorrow. The Federal Employee Benefits Open Season begins a week from tomorrow. OPM’s 2022 online FEHB Plan Comparison Tool is now available.
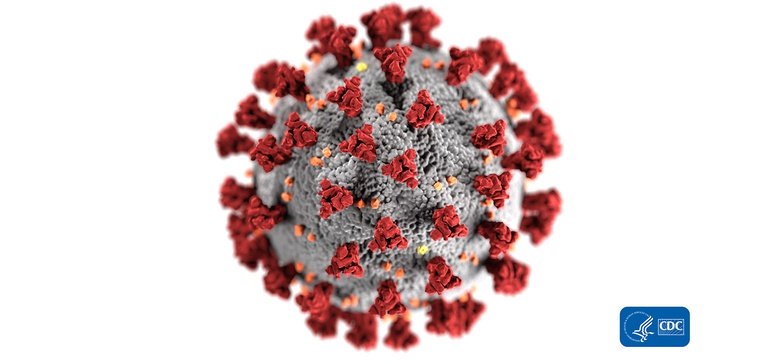
From the Delta variant front, the Wall Street Journal tells us that
The Food and Drug Administration is delaying a decision on Moderna Inc.’s application to authorize use of its Covid-19 vaccine in adolescents to assess whether the shot leads to a heightened risk of myocarditis, the company said.
The FDA notified Moderna on Friday evening that an analysis may not be completed until January of next year while the agency reviews recent international data on the risk of myocarditis after vaccination, the company said Sunday.
The Wall Street Journal reported earlier this month that the FDA was delaying a decision on Moderna’s application for authorization in 12- to 17-year-olds after several Nordic countries limited use due to myocarditis reports.
Moderna also said it would delay asking the FDA to authorize use of a lower dose of its shot in even younger children, ages 6 to 11, while the agency continues to review its request to clear the shots in adolescents.
From the CMS front, Medicare offers coverage for those under age 65 who are afflicted with End Stage Renal Disease (“ESRD”). On Friday, CMS finalized its ESRD prospective payment rule for calendar year 2022. In its announcement CMS explained that
Through the ESRD Prospective Payment System (PPS) annual rulemaking, CMS is making changes to the ESRD Quality Incentive Program (QIP) and the ESRD Treatment Choices (ETC) Model, and updating ESRD PPS payment rates. The changes to the ETC Model policies aim to encourage dialysis facilities and health care providers to decrease disparities in rates of home dialysis and kidney transplants among ESRD patients with lower socioeconomic status, making the model one of the agency’s first CMS Innovation Center models to directly address health equity.
“Today’s final rule is a decisive step to ensure people with Medicare with chronic kidney disease have easy access to quality care and convenient treatment options,” said CMS Administrator Chiquita Brooks-LaSure. “Enabling dialysis providers to offer more dialysis treatment options for Medicare patients will catalyze better health outcomes, greater autonomy and better quality of life for all patients with kidney disease.”
That makes sense to the FEHBlog.
From the healthcare network front, the Yale School of Public Health (YSPH”) informs use that “a new survey analysis from a researcher at the YSPH suggests that privately insured adults are significantly more likely to rate their mental health provider network as inadequate compared to their medical provider network.” With due respect to Yale, this finding is hardly surprising given the fact that relative few mental health therapists join a health plan network because they don’t need patient referrals. That’s why it so important for the hub and spoke telehealth services to offer ongoing mental health care over their networks.
From the OPM front, Federal News Network reports that
As agencies contemplate and continue to plan for the future of work, the Office of Personnel Management is trying to let agencies know they have some help — and some new resources — to guide them through the unknown.
The agency is preparing to release more guidance on telework and remote work “very soon,” OPM Director Kiran Ahuja said in an interview with Federal News Network.
It’s all part of an effort to help agencies establish themselves as model employers that can meet the moment — and part of OPM’s own plans to reestablish itself as a human capital resource for the rest of government. They’re priorities Ahuja set in the early days since becoming OPM director, and they’ll continue well into 2022 and beyond, she said.
The guide will offer, in some detail, advice for agencies on making the shift to remote and hybrid work.
“We want to support what’s involved in our lives around flexibilities and child care but also knowing that we can be really productive,” Ahuja said. “We have this guide coming out. We’re also pulling together trainings and information around how to manage in a hybrid work environment and how to operate well in a work environment, as well as a new website focused on future of work.”