Midweek update

Today, the FEHBlog attended day one of the virtual OPM AHIP FEHB Carrier Conference. OPM informed carriers to expect a carrier letter on the No Surprises Act. OPM also presented panels delving into Biden administration initiatives described in the 2023 call letter. The second and final day is tomorrow.
The FEHBlog suggests that OPM resume the practice of including health plan and PBM representatives on its conference panels to provide more relevant perspectives on these initiatives.
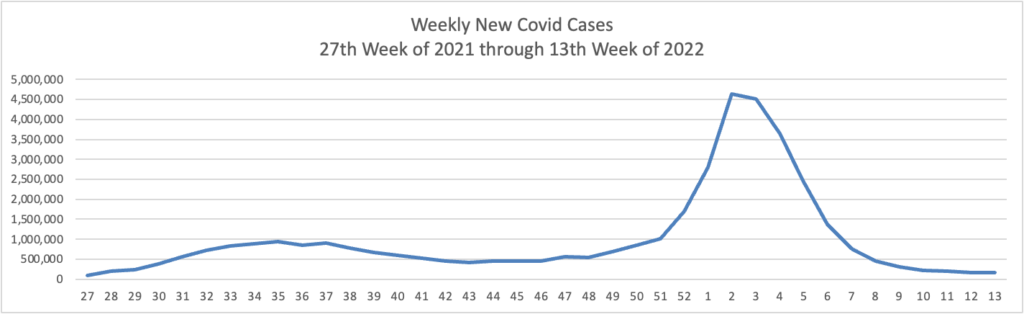
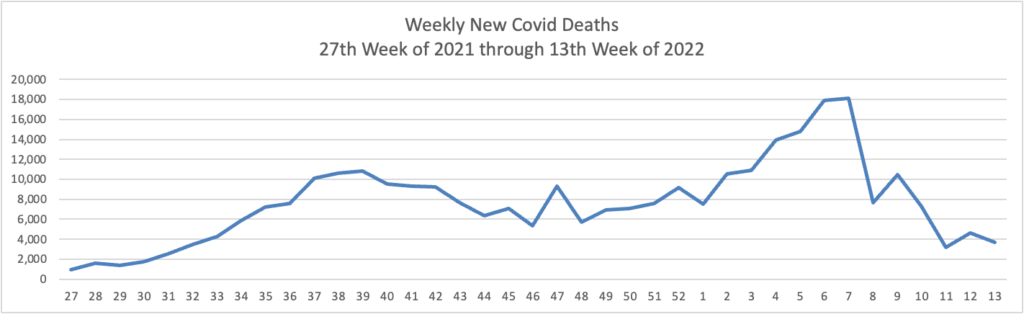
From the Omicron front, the Wall Street Journal informs us
There’s a good chance you’ll get Covid more than once.
Covid-19 reinfections are more common and can happen within a shorter window of time than doctors previously thought possible, recent research suggests. More than half of people in the U.S. showed signs of having been infected at least once as of February, according to a report Tuesday from the Centers for Disease Control and Prevention. * * *
“On average at a population level, the people who get reinfected have milder symptoms,” says Francois Balloux, an infectious disease epidemiologist and director of the UCL Genetics Institute in London. “That doesn’t mean that some people might not have a worse infection the second or even third time.”
From the SDOH front, Health Payer Intelligence tells us
The Blue Cross and Blue Shield Association (BCBSA) and the Blue Cross and Blue Shield companies have urged the healthcare industry to adopt national health equity data collection standards.
The companies released a paper that defines health equity and submits a proposed model for data collection standardization.
That is a valuable resource.
From the telehealth front, Healthcare Dive reports
Whether or not telehealth visits result in duplicative care — a hot topic on the Hill as Congress debates future telemedicine regulation — could depend on whether users have acute or chronic conditions, a new study suggests.
Researchers analyzed data from almost 41 million commercially insured adults, and found patients with acute conditions that had an initial telehealth visit were slightly more likely to have a follow-up encounter, emergency room visit or inpatient admission, compared to those who had an in-person visit.
However, patients with chronic conditions that had an initial telehealth visit were as or less likely to need follow-up care, than those with an initial in-person visit.
That’s practical information for you.
Healthcare Dive adds
Teladoc Health recorded a $6.6 billion impairment charge in the first quarter, reflecting the waning market value of its acquisition of chronic care company Livongo inked two years ago.
Teladoc, the largest virtual care company in the U.S., bought Livongo for $18.5 billion in cash and stock late 2020 in the biggest digital health deal to date. However, the merger has struggled, resulting in the large goodwill impairment charge for the Purchase, New York-based vendor.
The charge drove Teladoc’s net loss up to $6.7 billion in the quarter, a record for the company. That’s more than 33 times bigger than its loss of about $200 million during the same time last year; and about 16 times its full year 2021 net loss of $429 million.
Ouch.
The Wall Street Journal reports
Some of the nation’s largest pharmacies have blocked or delayed prescriptions over the last year from clinicians working for telehealth startups that have sprung up to treat attention-deficit hyperactivity disorder, according to pharmacies and people familiar with the issue.
The pharmacies in certain cases have expressed concerns that clinicians at Done Health and Cerebral Inc. are writing too many prescriptions for Adderall and other stimulants, the people said. The federal government considers the drugs controlled substances because of their potential for abuse and places them in the same category as cocaine.
From the mental health and substance use disorder front —
Fierce Healthcare calls attention to the fact
Mental and behavioral health conditions account for a growing segment of healthcare costs, and insurers have a significant opportunity to address these expenses and drive costs down overall, according to a new report [which is behind a Moody’s paywall].
Mental health conditions accounted for just 5.2% of healthcare spending in 2019, but the number of people with these conditions is expanding, particularly in the pandemic environment, according to a report from analysts at Moody’s Investors Service.
A recent study suggests that healthcare costs for people with behavioral health conditions are 3.5 times higher than for those without such conditions, according to the report. Annual healthcare costs for patients with behavioral health needs are $12,272, with just 7.9% of that specifically for the behavioral conditions.
The National Institutes of Health offers a Q&A with Dr. Rena D’Souza, the Director of the National Institute of Dental and Craniofacial Research.
RB: Thanks for joining me, Rena. Many people might not recognize the relevance of oral health in opioid use and pain. Can you give us some examples of NIDCR HEAL projects and recent findings?
RD: Rebecca, thanks for the opportunity to have this conversation. Managing and treating dental, oral, and craniofacial pain is central to NIDCR’s vision to improve oral health and well-being for all people. So there’s an obvious connection. NIDCR HEAL projects include research to discover new, non-addictive ways to prevent and treat orofacial pain disorders such as temporomandibular disorders, inflammatory and neuropathic pain, and oral cancer-associated pain. NIDCR HEAL researchers are also in the early stages of developing a material that can seal surgical wounds and deliver pain medicine on-site to help reduce the need for opioids after oral surgery. In addition, our institute is interested in how socioeconomic status, race, ethnicity, and other social determinants of health play a role in chronic pain, pain management, and patient outcomes.
This work is necessary to tackle our opioid epidemic.
The Department of Health and Human Services announced the availability of “new, free informational resources that inform Americans of their rights under law on coverage for mental health benefits.”
“The following resources have been posted on SAMHSA’s website:
- “Know Your Rights: Parity for Mental Health and Substance Use Disorder Benefits,” an updated trifold pamphlet explaining mental health parity, detailing what it means to the consumer, and listing the protections the parity law provides.
- “Understanding Parity: A Guide to Resources for Families and Caregivers,” which provides an overview of parity geared toward parents, family members or caregivers with information and tools to help them obtain behavioral health services for children or family members in their care.
- “The Essential Aspects of Parity: A Training Tool for Policymakers,” which provides state regulators and behavioral health staff an overview of mental health and substance use disorder parity and how to implement and comply with the federal parity law regarding employer-sponsored health plans and group and individual health insurance.”