King Day Weekend Update
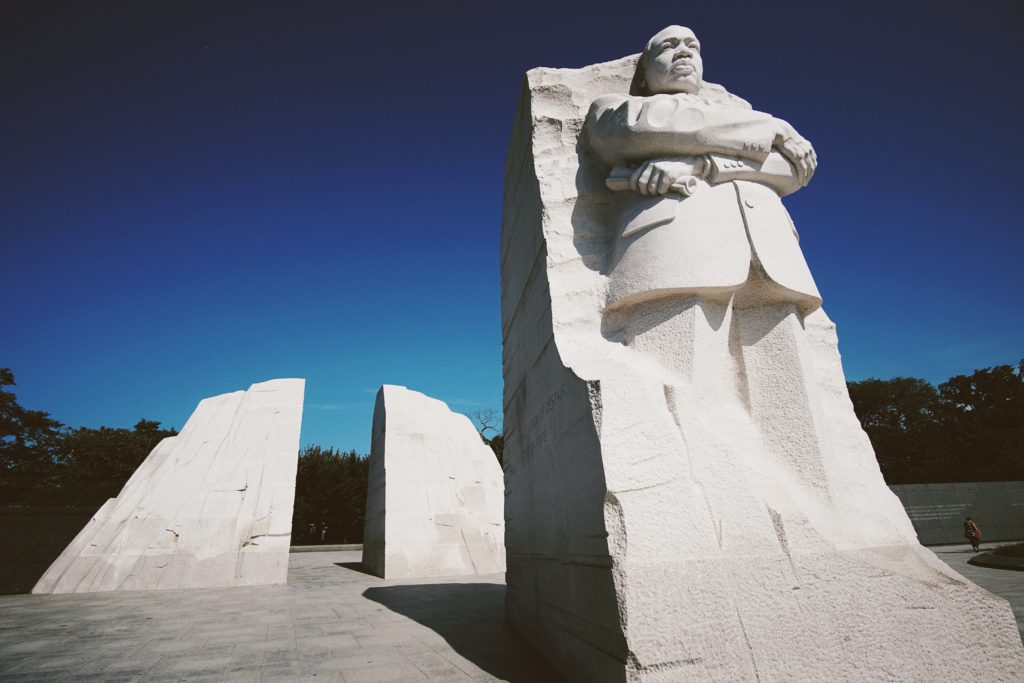
Happy King Day. Dr. King would have been 95 years old today.
From Washington DC,
- The House of Representatives and the Senate are in session on Capitol Hill this week (except for today’s holiday.) Here is a link to the Committee hearing schedule.
- Roll Call adds
- “House and Senate leaders have agreed to extend temporary government funding in two batches, through March 1 and March 8, according to a source familiar with the plan.
- “The decision comes as lawmakers face a Friday, Jan. 19 deadline to clear a temporary spending bill for four of the dozen annual appropriations bills — Agriculture, Energy-Water, Military Construction-VA and Transportation-HUD. The remaining eight bills’ stopgap funds expire after Feb. 2 under the most recent interim spending law.”
- The Wall Street Journal reports,
- Medicare patients lining up to fill pricey prescriptions at the pharmacy counter this year will realize some good news: For the first time, there is a ceiling on how much they will pay in 2024 for their Part D drugs.
- Changes brought about by the 2022 Inflation Reduction Act mean that people on Part D plans now pay no more than roughly $3,300 on drugs annually—a number that could shift a bit based on whether they take brand or generic medications. In 2025, that cap will change again to a flat $2,000.
- Patient Engagement HIT informs us,
- “Transportation access continues to be a leading social determinant of health, with new CDC data showing it affected 5.7 percent of adults over the course of 12 months.
- “The report, which used 2022 data, also showed that women were more likely than men to face transportation access barriers, with 6.1 percent and 5.3 percent reporting as much, respectively. * * *
- “Younger adults rather than older adults, for example, were more likely to face challenges related to transportation access, with 7 percent of 18-34-year-olds reporting problems compared to 4.5 percent of those over age 65. Odds of transportation-related barriers decreased with age, the CDC researchers said.
- “Moreover, racial disparities persisted, with American Indian/Alaska Native adults being the most likely to report a lack of reliable transportation. Of those respondents, 17.1 percent said they faced barriers in the previous 12 months.
- “That compares to 9.2 percent of Black respondents, 7.6 percent of other or multiple-race respondents, 6.9 percent of Hispanic respondents, 4.8 percent of White respondents, and 3.6 percent of Asian respondents who said the same.”
From the public health and medical research front,
- The Washington Post and Consumer Reports tell us “How to prevent shingles and what to do if you get it.”
- “Shingrix, a two-dose shingles vaccine that was approved by the Food and Drug Administration in 2017, can reduce the incidence of shingles and its complications significantly. “The vaccine, the one we have available today, is spectacularly effective,” says William Schaffner, an infectious-disease specialist at Vanderbilt University Medical Center in Nashville.
- “But only about 30 percent of adults eligible for this vaccine have gotten it, according to 2022 report by the Government Accountability Office. If you’re wondering about the effects and risks of shingles and whether Shingrix is right for you, [the article provides] what you need to know.
- The New York Times reports,
- “Marijuana is neither as risky nor as prone to abuse as other tightly controlled substances and has potential medical benefits, and therefore, should be removed from the nation’s most restrictive category of drugs, federal scientists have concluded.
- “The recommendations are contained in a 250-page scientific review provided to Matthew Zorn, a Texas lawyer who sued Health and Human Services officials for its release and published it online on Friday night. An H.H.S. official confirmed the authenticity of the document. * * *
- “President Biden urged federal officials to “expeditiously” re-examine marijuana classification in October 2022, when he also issued pardons for those charged with marijuana possession under federal law.”
- Fortune Well identifies “seven immune-boosting foods to eat when you’re sick with COVID or flu.”
From the U.S. healthcare business front
- Benefits Pro points out,
- “A new report from Humana finds that “value-based care,” which focuses on quality of care and patient experience with deeper patient engagement, that is provided to Medicare Advantage members kept patients healthier and lowers costs.
- “The new report is part of an annual assessment of the model, which stresses a more personal approach, more time spent with patients, and more coordinated care than traditional fee-for-service models of care. The model also puts an emphasis on prevention and lifestyle changes to help patients manage their health.
- “The tenth-annual report on the efficacy of the value-based model for Medicare Advantage members noted that the U.S. health system has faced some significant challenges in recent years, including the COVID pandemic, a stressed workforce, and growing awareness of inequities in health care. The Humana analysis acknowledges challenges remain but found better scores on measurements across the board for patients in the value-based care model.”
- Per Forbes,
- “On November 13, 2023, women’s health advocates – including entrepreneurs and investors – celebrated a positive step forward for the industry; that day, the White House announced the first-ever Initiative on Women’s Health Research. The goal of the Initiative is to engage the federal government and private and public sectors to fund women’s health, spur innovation, close research gaps, and improve diagnosis, disease prevention, education, treatment, and more.
- “This Initiative, however, was not the only new and noteworthy event in women’s health recently. In 2023 alone, women’s health startups saw gains in their average deal sizes, in the percentage of healthcare venture capital funding they raised, and in the attention they received. If these trends continue, 2024 could be the long-awaited and much-needed transformative year, bringing attention, capital, and recognition to this historically overlooked, underinvested, and undervalued space.”







