New OPM Director plus Tuesday’s Tidbits

The Senate narrowly confirmed Kiran Ahuja to be Office of Personnel Management Director this afternoon. Here’s the Senate play by play from the Senate Press Gallery website.
1:37 p.m. Cloture was invoked on the Ahuja nomination, 51-50. Vice President Harris broke the tie.
2:26 p.m. Senator Peters spoke in support of the Ahuja nomination.
2:30 p.m. The Senate began a vote on confirmation of Executive Calendar #107 Kiran Arjandas Ahuja to be Director of the Office of Personnel Management for a term of four years.
3:26 p.m. By a vote of 51-50, the Senate confirmed Executive Calendar #107 Kiran Arjandas Ahuja to be Director of the Office of Personnel Management for a term of 4 years. The Vice President cast the tie breaking vote.
Here is a link to Ms. Ahuja’s Wikipedia page. Here are links to the Federal Times, Govexec and Federal News Network reports on this event. The FEHBlog wishes Ms. Ahuja good luck.
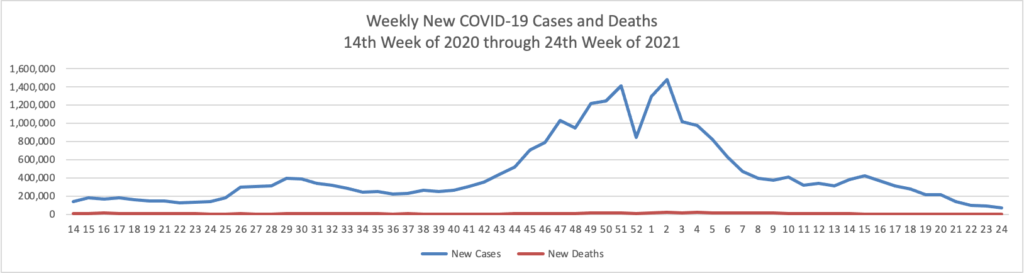
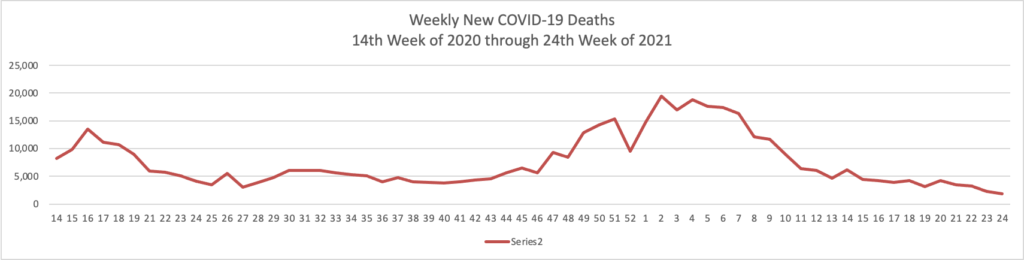
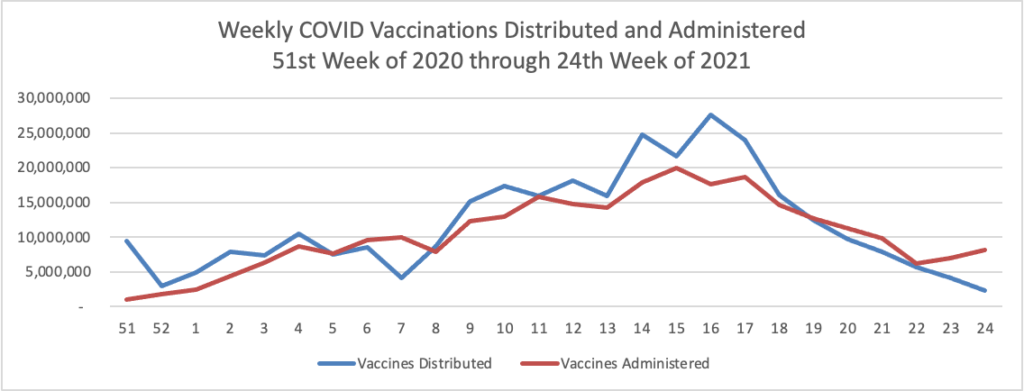
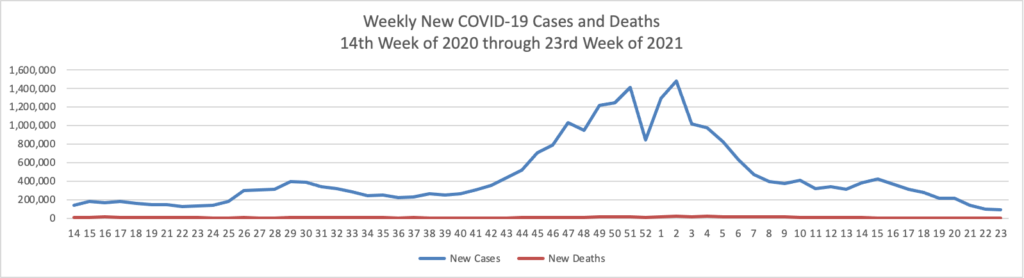
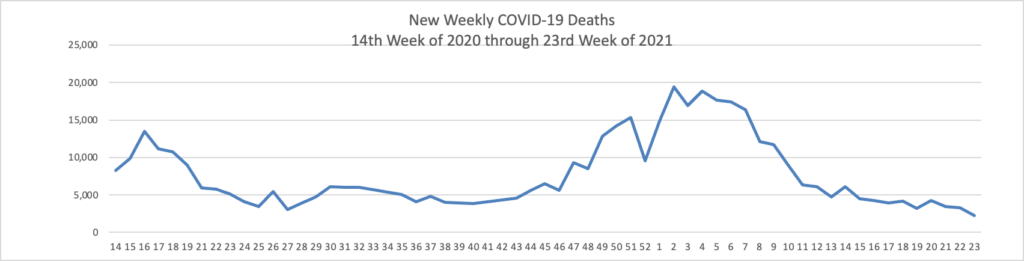
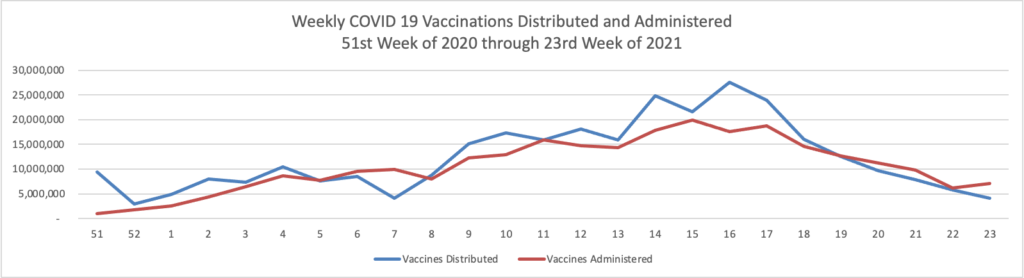
The Senate Health Education Labor and Pensions Committee held a hearing on COVID-19 vaccination efforts today. Here is a link to the Sen. Patty Murray’s (D Wash) statement on the hearing. Sen. Murray is the Committee chair.
In this regard, the Wall Street Journal reports that
The White House said the U.S. will fall short of President Biden’s goal for 70% of the adult population to receive at least one coronavirus vaccine dose by July 4.
Mr. Biden had set the goal in early May, with an aim for a return to normalcy to mark the Independence Day holiday. White House Covid-19 coordinator Jeffrey Zients said Tuesday the target had been met for those age 30 and over but not for the overall eligible population.
Mr. Zients said it would take a few extra weeks to reach the president’s target and cited a reluctance to get the vaccine among people between the ages of 18 and 26 as one of the challenges facing the country.
“The reality is many younger Americans have felt like Covid-19 is not something that impacts them and they have been less eager to get the shot,” Mr. Zients said.
On Thursday, June 24, at 10 am, the Financial Services and General Government Subcommittee of the House Appropriations Committee will markup the fiscal year 2022 appropriations bill that includes OPM and FEHB appropriations. Here’s a link to a Fedweek article on the markup.
STAT News offers a couple of sobering articles, one on antibiotic resistance and the other on health equity concerns
- According to a new STAT Report an estimated 700,000 people die annually from antimicrobial resistance, a number that could rise to 10 million by 2050, according to a World Health Organization report issued in 2019. In the U.S. alone, there are more than 2.8 million antibiotic-resistant infections and 35,000 deaths from those infections each year, according to data from the Centers for Disease Control and Prevention. A number of issues have fueled resistance and stunted development of new antibiotics. And while there are various efforts underway to address those challenges, creating incentives to change the trajectory of antibiotic resistance takes commitment and imagination. There are several experiments under way that aim to spur development of new products while still ensuring profit. In the U.K. and Sweden, pilot programs are testing a pull incentive, which involves a subscription-style business model in which a government offers upfront payments to drug makers in exchange for unlimited access to their antibiotics. The idea is to enable drug companies to recover their costs and make an appropriate profit without having to sell large volumes of antibiotics. Last week, U.S. lawmakers re-introduced legislation to create a similar mechanism.
- [Researchers have identified]232 counties in the mainland U.S. where men aged 49 and under are at unusually high risk of dying from colorectal cancer, according to a study published last year in the American Journal of Cancer Research. The researchers also found that compared with white men, Black men in these hot spots who have colorectal cancer are more likely to be diagnosed with advanced stages of the disease and less likely to survive it. * * * [S]ince the 1990s, even as colorectal cancer rates have declined for people 50 and older, they have more than doubled among American adults under 50, according to the National Cancer Institute. By 2030, predicts a study published in April, colorectal cancer will be the leading cause of cancer-related deaths in people aged 20 to 49. The reason behind the rise remains a mystery. “We don’t know where this is coming from,” said Charles R. Rogers, an assistant professor of public health at the University of Utah School of Medicine and lead author of the hot spots study. “Just like we don’t really know why Black people have the highest chance of getting and dying from it.” The article explains how researches like Professor Rogers are shedding light on the cause of this inequity by studying the hot spots, among other things.
In brighter Tuesday Tidbits
- The Patient Centered Outcomes Research Institute funded by health plan premiums is seeking public comment on its national health priorities. The public comment period runs from June 28 through August 27.
- Fierce Healthcare reports that “Five Blues plans are teaming up to invest in a new pharmacy solutions venture called Evio. Blue Cross Blue Shield of Massachusetts, Blue Cross Blue Shield of Michigan, Blue Shield of California, Highmark Health and Independence Blue Cross are backing Evio, according to an announcement released Tuesday. The new company aims to establish outcomes-based arrangements with drugmakers, especially for high-cost therapies. In addition, Evio aims to collect and provide real-world evidence for medications to ensure the right product is getting to the right patient.” Makes sense to the FEHBlog.
- Fierce Healthcare also informs us that “Amazon Web Services wants to help incubate early-stage digital health companies that can collaborate with the tech giant’s healthcare customers and partners. Amazon’s cloud division launched a healthcare accelerator to boost startups’ growth in cloud technologies and enable early-stage companies to tap into AWS’ technical and commercial expertise. The program will focus on technologies such as remote patient monitoring, data analytics, patient engagement, voice technology and virtual care, according to a blog post from Sandy Carter, vice president of worldwide public sector partners and programs at AWS.”