OPM Director Ahuja Celebrates Her First Year

U.S. Office of Personnel Management Director Kiran Ahuja celebrated her first year in office today. Here are links to an OPM press release and a Govexec account of Director Ahuja’s press conference.
The press release identifies her “major accomplishments with respect to the FEHB Program as
- Providing health benefits that are responsive to employee needs
- All Federal Employee Health Benefits (FEHB) carriers provide telehealth services ensuring access to health providers during the pandemic and on an ongoing basis going forward. In a 2021 survey, 43% of FEHB enrollees report using telehealth benefits and use was greatest among those with mental health or behavioral health concerns.
- In accordance with EO 14035, which directed OPM to promote equitable healthcare coverage and services for enrolled LGBTQ+ employees and their covered family members through the FEHB Program, OPM prioritized and strongly encouraged FEHB Carriers to provide gender-affirming care benefits consistent with standards published by recognized medical experts.
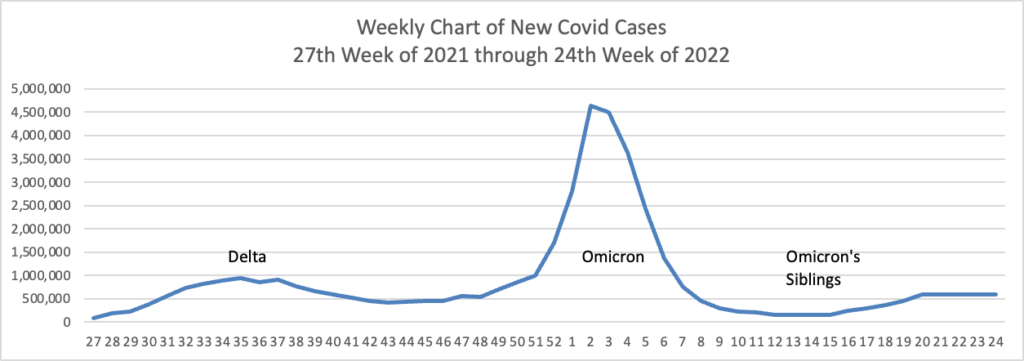
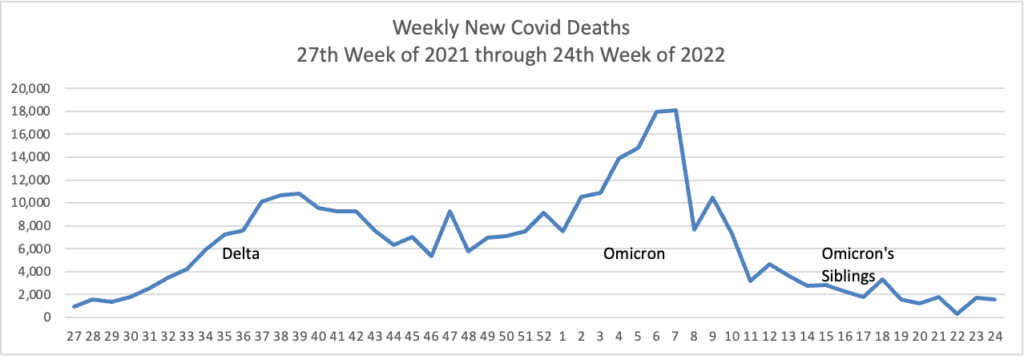
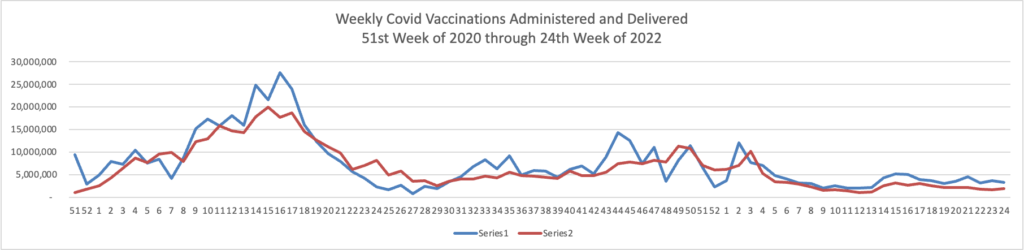
From the Omicron and siblings front
The Wall Street Journal reports
- Advisers to the Centers for Disease Control and Prevention (ACIP) backed use of Moderna Inc.’s Covid-19 vaccine in children ages 6 to 17 years.
- Children in the age group already have access to Covid-19 vaccines made by Pfizer Inc. and its partner BioNTech SE. The advisers recommended on Thursday that Moderna’s shot should also be made available to that age range, in a pair of 15-0 votes.
- The advisers’ endorsement follows the Food and Drug Administration’s authorization of the shots last week. It is one of the last steps before the Moderna shot would be more broadly available in doctors’ offices, pharmacies and vaccine clinics.
Other news reports indicate that CDC Director Walensky is expected to endorse this recommendation late Thursday or Friday.
MedPage Today informs us
A fourth dose, or second booster, of Pfizer/BioNTech’s COVID-19 vaccine (Comirnaty) protected seniors living in long-term care from the most severe outcomes during the Omicron wave, despite showing a more limited effect against infection, according to prospective data from Israel.
Among over 40,000 residents, effectiveness of a fourth dose (versus a third given at least 4 months prior) was 64% and 67% against hospitalizations for either mild/moderate or severe illness, respectively, and 72% against COVID-19-related deaths, reported Khitam Muhsen, PhD, of Tel Aviv University in Israel.
From the conference front, Fierce Healthcare offers the following articles on this week’s AHIP conference:
- SDOH — “As the healthcare industry grapples with health inequities and disparities across the country, health insurers are well-positioned to lead the charge, experts said Wednesday.”
- Biosimilars — “[I]t is important to note that while the competition generated by these new launches can help lower payer costs—depending on pricing and available discounts—biosimilars may not necessarily be the lowest cost option in all therapeutic categories.”
- Behavioral health — “As the team at Cigna’s Evernorth builds its strategy around behavioral health, it’s focusing on a key throughline: simplicity.”
From the Rx coverage front —
- The Senate Commerce Committee announced clearing for Senate floor consideration the Committee leadership’s PBM transparency bill (S 4293). The vote in favor of floor consideration was 19-9. Fierce Healthcare offers an article on the Committee’s action.
- STAT News reports on a bipartisan Senate proposal to control insulin prices by locking in current manufacturer profits. “David Mitchell, founder of Patients for Affordable Drugs, a patient advocacy group that doesn’t accept funds from the pharmaceutical industry, called the bill “disappointing,” and said it would just shift costs to patients in other ways. ‘It’s pharma’s preferred solution to drug pricing,’ Mitchell said.”
- STAT News also tells us that “In response to rising prices for medicines, public and private payers increasingly rely on assessments of cost-effectiveness to justify coverage. But a new examination finds that such studies sponsored by drug companies were often biased in favor of setting higher prices for their medicines.” The study was published in the BMJ.
- The FDA released an “Action Plan for Rare Neurodegenerative Diseases, Including ALS “(also known as Lou Gehrig’s Disease).
In other vaccine news, AHIP informs us that
ACIP additionally voted [today[ to recommend adults aged 65 and older preferentially receive any one of the following higher dose or adjuvanted influenza vaccines: quadrivalent high-dose inactivated influenza vaccine (HD-IIV4), quadrivalent recombinant influenza vaccine (RIV4), or quadrivalent adjuvanted inactivated influenza vaccine (aIIV4); however there is no preference between these three vaccines.
The Committee also recommended that pneumococcal vaccine PCV15 may be used as an option to PCV13 for children aged under 19 years according to currently recommended PCV13 dosing and schedule. ACIP voted that Priorix (GSK) be used, as an option, to prevent measles, mumps, and rubella, in accordance with currently recommended schedules and off-label uses
MedPage Today reports good vaccination news
Overall rates of human papillomavirus (HPV) vaccination among adolescents increased by nearly 20% over a 5-year period, according to survey data.
Among teens ages 13 to 17, overall HPV vaccine coverage increased from 56.1% in 2015 to 75.4% in 2020, and rates for those completing the full vaccine series jumped from 40.3% to 59.3%, respectively, reported Peng-jun Lu, MD, PhD, of the CDC in Atlanta, and colleagues
“CDC’s latest data show that HPV vaccination coverage among adolescents is increasing, which is important to prevent HPV infections that can lead to several cancers in both females and males,” Lu told MedPage Today.
The authors also noted that a doctor’s recommendation was correlated with greater willingness to receive the vaccine. Of those who were advised to get vaccinated, 80.7% received vaccination compared with 51.7% who were given no such advice. These findings mirrored another study, which found that provider recommendations boosted HPV vaccination rates among kids ages 11 to 12.
Well-child visits were also associated with higher rates of vaccination. Among kids ages 11 to 12, 80.3% who had a visit were vaccinated compared with 64.8% who did not have a visit.
From the nicotine front, the New York Times reports
The Food and Drug Administration on Thursday ordered Juul to stop selling e-cigarettes on the U.S. market, a profoundly damaging blow to a once-popular company whose brand was blamed for the teenage vaping crisis. The order affects all of Juul’s products on the U.S. market, the overwhelming source of the company’s sales.
Juul is considering its legal options.