Happy Winter Solstice

Winter is not only coming; winter is here.
From Capitol Hill, the Wall Street Journal reports
Senators were bracing for a late night in the Capitol, as the timing of votes on the $1.65 trillion omnibus spending bill and possible amendments remained uncertain and the Friday night deadline to avoid a government shutdown crept closer.
The Senate could start voting on amendments later Wednesday, teeing up a late night or early morning of voting, even as they also attend an address to Congress in the evening by Ukrainian President Volodymyr Zelensky. Adding to the pressure, senators are looking to get out of town ahead of winter storms expected in coming days.
“We’re still working on an agreement to vote on amendments and pass the omnibus tonight,” Senate Majority Leader Chuck Schumer (D., N.Y.) said Wednesday night. “We aren’t there yet, we’re making progress.” Once the Senate passes the measure, it would move to the House, which is expected to approve it quickly.
Politico Pulse, STAT News, and the Washington Post offer follow-up stories on the healthcare provisions in the omnibus. Of note, the Washington Post confirms
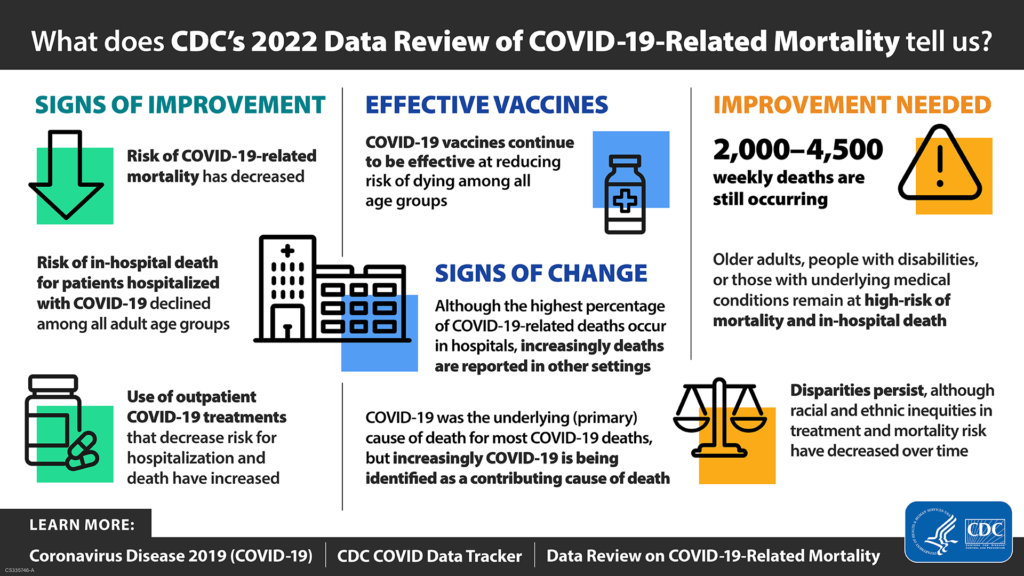
Congress again rebuffed the White House’s request for new dollars to combat the coronavirus. Last month, Biden administration officials urged lawmakers to approve about $9.25 billion in emergency funds to help ensure access to vaccines and treatments while supporting new research into long covid.
The battle over more funds has been ongoing since the spring, and Republicans have refused to budge, with one Senate GOP aide telling The Health 202 that they want further explanations on how the federal government has spent billions previously allocated for its pandemic response.
Politico Pulse adds
A long list of measures aimed at tackling the ongoing opioid crisis is in the bill, including $1,575,000,000 in state grants to go toward substance abuse prevention and treatment. It also incorporates significant provisions of the Mainstreaming Addiction Treatment Act, including the elimination of a DEA requirement that clinicians get an extra certification to prescribe buprenorphine, and the NOPAIN Act, which improves access to FDA-approved non-opioid therapies for outpatient surgical procedures.
STAT News explains how the omnibus breathes new life into Medicare’s hospital-at-home program.
What’s more, this week the Senate confirmed the nominations of Rob Schriver to be OPM Deputy Director and Richard Revesz to be director of OMB’s Office of Information and Regulatory Affairs.
From the judicial front –
- The Society for Human Resource Management tells us, “The 5th U.S. Circuit Court of Appeals recently ruled that the federal government cannot enforce a COVID-19 vaccine mandate on federal contractors. The court’s Dec. 19 decision found that the Biden administration overstepped its authority with the vaccine mandate.”
- Healthcare Dive discusses the latest hearing before Judge Kernodle in the second Texas Medical Association challenge to the No Surprises Act independent dispute resolution rule. The FEHBlog finds this to be a premature lawsuit at best.
From the public health front
- The Wall Street Journal reports
The nose knows why some people still can’t smell long after recovering from Covid-19.
A haywire immune response in the olfactory system was found to explain why some people still can’t smell long after symptoms of the disease have abated, according to a small, peer-reviewed study published Wednesday in the journal Science Translational Medicine. In some cases, the immune or inflammatory response was detected in patients with smell loss up to 16 months after recovery from Covid-19.
Compared with people who can smell normally, patients with long-term smell loss had fewer olfactory sensory neurons, cells in the nose responsible for detecting smells and sending that information to the brain. Patients with lingering loss of smell had an average of 75% fewer of the neurons compared with healthy people, said Brad Goldstein, a study co-author and sinus surgeon at Duke University.
“We think the reduction of sensory neurons is almost definitely related to the inflammation,” Dr. Goldstein said.
- HHS announced “making an additional supply of Tamiflu available to jurisdictions to respond to an increased demand for the antiviral during this flu season, including through the Strategic National Stockpile (SNS). Jurisdictions will work with their ASPR Regional Teams to evaluate any requests for Tamiflu through the SNS, ensuring that states, territories, and tribes receive the assistance they need without affecting our nation’s preparedness for a future pandemic flu.”
- Beckers Hospital Review discusses how five payers are addressing maternal health.
- A JAMA article examines whether “the new CDC Opioid Prescribing Guidelines will help correct the course in pain care.”
From the drug development and distribution front
The Institute for Clinical and Economic Research “posted its revised Evidence Report assessing the comparative clinical effectiveness and value of the following treatments for multiple sclerosis (MS):
Monoclonal Antibodies
- natalizumab (Tysabri®, Biogen)
- ofatumumab (Kesimpta®, Novartis)
- ocrelizumab (Ocrevus®, Genentech)
- rituximab (Rituxan®, Genentech, and biosimilars)
- ublituximab (TG Therapeutics)
Oral Therapies
- dimethyl fumarate (Tecfidera®, Biogen, and generics)
- diroximel fumarate (Vumerity®, Biogen)
- monomethyl fumarate (Bafiertam®, Banner Life Sciences)
- fingolimod (Gilenya®, Novartis)
- ozanimod (Zeposia®, Bristol Myers Squibb)
- ponesimod (Ponvory®, Janssen)
- siponimod (Mayzent®, Novartis)
- teriflunomide (Aubagio®, Sanofi)
Science reports,
As enthusiasm mounts for a new experimental antibody that appears to slow cognitive decline in some Alzheimer’s patients, a third death linked to the drug during its clinical testing may amplify concerns about its safety. Science has obtained medical records showing a 79-year-old Florida woman participating in an ongoing trial of the antibody died in mid-September after experiencing extensive brain swelling and bleeding, as well as seizures. Multiple neuroscientists who reviewed the records at Science’s request believe her death was likely caused by the antibody, lecanemab.
“The brain swelling and the microhemorrhages … could be a serious side effect of the study medication,” and should be evaluated by trial investigators, says Ellis van Etten, a neuroscientist and neurologist at Leiden University.
Biopharma Dive informs us
- Pfizer has started dosing patients in a Phase 2 study of its entry into a closely watched class of drugs for treating diabetes and obesity.
- The dosing of the first patient with the drug, dubbed PF-07081532, triggered a $10 million payment to partner Sosei Heptares, the Japanese drugmaker said Wednesday. Pfizer scientists working with Sosei’s technology discovered the medicine, and Pfizer is responsible for developing it.
- Pfizer aims to bring a once-daily oral treatment into a class of medicines known as GLP-1 agonists, which stimulate the body to produce insulin by acting on natural body hormones known as glucagon-like peptides. Most of the approved GLP-1 agonists must be injected.