Weekend Update

Congress is back in session this week for Committee business and floor voting. The Senate calendar notes the cloture motion on the Postal Reform Act of 2022 ripens tomorrow February 28 at 5:30 pm. This means that the Senate can hold a cloture vote on the bill later that evening or the following business day. A cloture vote requires 60 votes in favor.
We are eleven days away from the end of the current continuing resolution funding the federal government. That deadline will grab Congress’s attention.
The President will give his State of the Union address on Tuesday, March 1.
From the No Surprises Act (NSA) front, Prof. Katie Keith breaks down the Texas Medical Association decision rendered last Wednesday in the federal district court for the Eastern District of Texas. At stake were the provisions in the second interim final rule implementing the NSA that the independent dispute resolution entity acting as the arbitrator to resolve payment disputes between health plans and certain out-of-network provider accept the plan’s statutory payment known as the Qualifying Payment Amount “unless a party submits credible information that clearly demonstrates that the QPA is materially different from the appropriate out-of-network rate.”
On February 23, Judge Kernodle * * * issued a decision and final judgment vacating provisions of the interim final rule related to the “rebuttable presumption.” He held that the plaintiffs had standing to challenge the rule, that the rule is inconsistent with the NSA, that the federal agencies should not have bypassed notice and comment procedures, and that the challenged provisions should be vacated and remanded to the agencies for revisions. The vacated provisions, listed here, are:
— The requirement that the IDR entity select the offer closest to the QPA unless there is credible information to demonstrate that this is not the appropriate rate;
— The requirement that “additional information” clearly demonstrate that the QPA is materially different from the out-of-network rate;
— The definition of “material difference;”
— All four examples on how IDR entities should choose between competing offers; and
— The requirement that the IDR entity explain why it chose an offer not closest to the QPA.
As you can see, this is a relatively surgical approach; these are the only provisions in the rule that have been invalidated. But these are important provisions designed to ensure a well-functioning, predictable IDR process and help hold down health care costs and premiums.
Professor Keith adds
Judge Kernodle rejected [the federal government’s] requests for limited relief. Instead, he vacated the challenged provisions on a nationwide basis with a sweeping assertion that “there is nothing the Departments can do on remand to rehabilitate or justify the challenged portions of the Rule as written. * * *
From here, DOJ will presumably appeal Judge Kernodle’s decision to the Fifth Circuit and perhaps request a stay while the case is on appeal. If a stay is not granted, the court’s decision remains in effect, meaning the IDR provisions noted above are unlawful and set aside. The IDR process will still be available and is expected to begin in earnest in March 2022. But the ruling increases the risk that some providers will try to leverage the federal IDR process to obtain higher rates than are warranted, potentially leading to higher health care costs and premiums.
What’s more,
Federal officials have already indicated that they will issue a final IDR rule by May 2022 and will likely be reviewing Judge Kernodle’s decision with an eye towards whether the final rule can include provisions that are similar to those in the interim final rule—as well as whether to rescind or replace the challenged provisions. The final rule will likely affect the timeline of current litigation and perhaps trigger future lawsuits.
It’s not a pretty picture for health plans at this point.
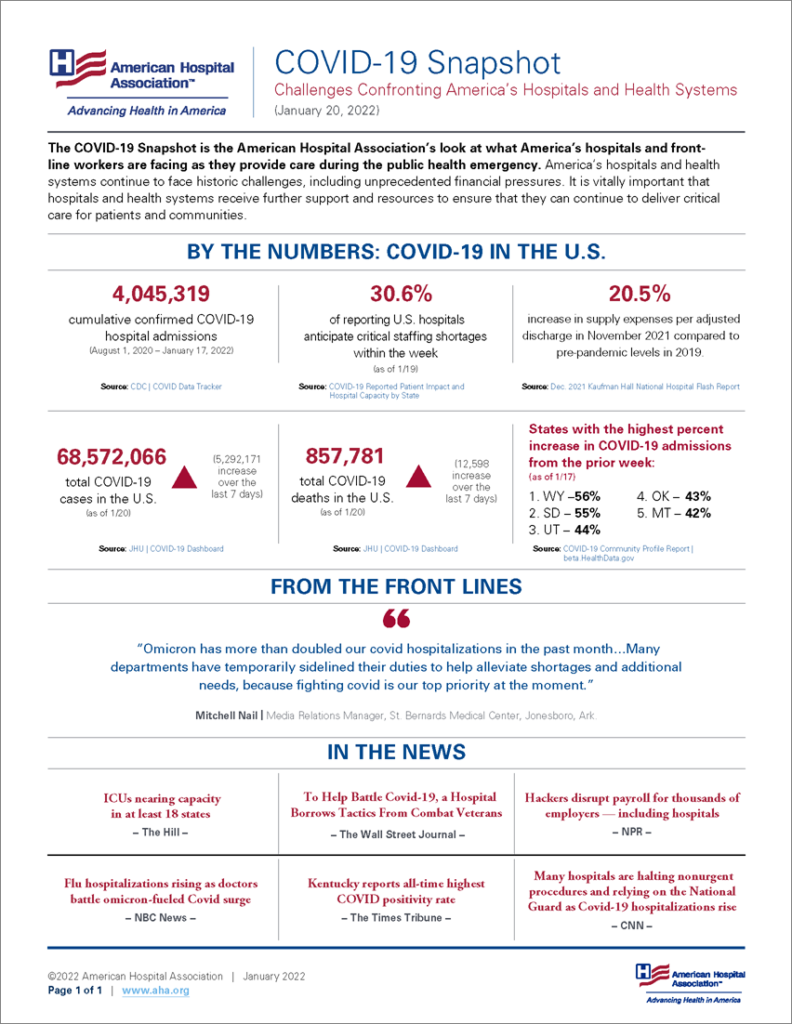
From the Omicron front, the Wall Street Journal discusses the steps that government agencies and public health organizations are taking to make rapid at home Covid tests available and understandable to the most vulnerable of us, “including low-income areas, rural parts of the country and some communities of color.”
From the behavior health care front, Health Payer Intelligence tells us
AHIP called on providers and policymakers to join payers in their efforts to integrate behavioral healthcare and physical healthcare in an issue brief on the subject.
The payer organization laid out three critical strategies for integrating behavioral healthcare.
The collaborative care model (CoCM) uses care management to facilitate patient-centered care, and many of its services are recognized and reimbursed by CMS.
The expanded and integrated care management model uses care management to support individuals with chronic conditions, specifically behavioral healthcare conditions. The model leans on screening tools in the primary care environment to identify conditions earlier.
Finally, the value-based purchasing and alternative payment models incentivize whole-person care financially. However, outcomes-based payment is challenging to measure in behavioral healthcare.
This is straight path to federal mental health parity compliance. Thanks AHIP.
From the OPM front —
- Fedscoop lists the important links on the OPM website for federal and Postal employees considering retirement or about to retire.
- Govexec discusses a recent GAO report on an OPM information technology project to overhauls it financial system for managing the government’s fringe benefit programs, including the FEHB.
From the good works department, Fierce Healthcare reports
Health Care Service Corporation [a Blue Cross licensee] is teaming up with the National Fitness Campaign to open outdoor fitness centers in Illinois and Texas.
The insurer will invest $850,000 to open 35 Fitness Courts across both states, according to an announcement. Construction is set to begin this summer, with the goal of opening the first locations in the fall.