Midweek Report

From Washington, DC,
- Federal News Network interviews Stephanie Kostro, executive vice president for policy at the Professional Services Council about the re-write of the Federal Acquisition Regulation that the President announced in an April 16, 2025, Executive Order.
- Federal News Network adds,
- “After laying off employees as part of its reduction in force (RIF), the Office of Personnel Management is now circulating a handful of job announcements to impacted employees that are nearly identical to their previous roles — only in a different OPM component.
- “In an internal email obtained by Federal News Network, OPM notified the impacted staff members on Monday of five vacancies in OPM’s Human Resources Solutions (HRS) office, which manages the software for USA Jobs, USA Staffing and other federal HR products and services.”
- Fierce Healthcare tells us,
- “The National Institutes of Health (NIH) will begin work on a comprehensive federal database of patient records to study autism and chronic disease, Director Jay Bhattacharya, M.D., Ph.D., announced Monday.
- “The commitment gives legs to Department of Health and Human Services (HHS) Secretary Robert F. Kennedy Jr.’s calls to find the root cause of childhood autism, which he calls an epidemic. The NIH appears poised to put federal resources to work to create a central, shareable resource for the researchers that undertake RFK Jr.’s call to action.”
From the judicial front,
- Healthcare Dive informs us,
- “U.S. Bankruptcy Judge Stacey Jernigan approved Prospect Medical Holdings’ plan to begin winding down operations at Crozer Health on Tuesday, after lawyers for the health system said an 18 months-long effort to find new buyers for the facilities was unsuccessful.
- “Emergency departments at Crozer-Chester Medical Center and Taylor Hospital, both in Delaware County, Pennsylvania, are set to stop receiving patients by ambulance this week. They’ll continue to accept walk-in patients for up to a week after, according to the hospitals’ closure plan, which attorneys characterized as evolving.
- “The closure plan faced significant pushback from county officials, nurses and nonprofits who warn that closing the facilities will force residents to travel farther for care and could risk lives.”
- STAT News reports,
- “Amid ongoing battles over alternate supplies of blockbuster weight loss drugs, Eli Lilly filed new lawsuits against four telehealth firms and their affiliates but is using a new line of attack — the drugmaker accused two of the companies of engaging in the corporate practice of medicine.
- “To date, Lilly and its rival, Novo Nordisk, have filed dozens of suits against numerous companies involved in compounding versions of semaglutide and tirzepatide, the obesity and diabetes drugs known as GLP-1s. For the past three years, telehealth firms, compounding pharmacies, and med spas have partnered to manufacture, prescribe and distribute copies of the drugs while shortages existed. Those lawsuits alleged trademark infringement, false claims and unfair competition, but have so far yielded varying outcomes.
- “This time, Lilly has alleged two companies, Mochi Health and Fella Health, engaged in the corporate practice of medicine, which refers to controlling and influencing prescribing decisions of health care providers. They purportedly did so with the help of affiliated medical groups and compounding pharmacies, according to separate lawsuits filed on Wednesday in the U.S. District Court for the Northern District of California.”
From the public health and medical research front,
- The American Hospital Association News points out,
- “U.S. births grew 1% in 2024 to 3.6 million, according to preliminary data from the Centers for Disease Control and Prevention. The cesarean delivery rate slightly increased to 32.4% in 2024, from 32.3% in 2023. The 2024 preterm birth rate was 10.41%, unchanged from 2023.”
- and
- “There have been 8,064 reported cases of whooping cough in the U.S. so far this year, according to the latest data from the Centers for Disease Control and Prevention. There were 3,835 cases at the same time in 2024.”
- “There have been 8,064 reported cases of whooping cough in the U.S. so far this year, according to the latest data from the Centers for Disease Control and Prevention. There were 3,835 cases at the same time in 2024.”
- Per today’s American Medical Association’s Morning Rounds,
- “The New York Times (4/22, Gross) reports that “neuroscientists have learned that estrogen is vital to healthy brain development but that it also contributes to conditions including multiple sclerosis and Alzheimer’s. Changes in estrogen levels – either from the menstrual cycle or external sources – can exacerbate migraines, seizures and other common neurological symptoms.” In the brain, “estrogen can bind directly to receptors within neurons and other cells, setting off a cascade of actions. It can also be broken down into metabolites, called neurosteroids, which exert their own far-reaching effects.” Researchers also know that estrogen “can modulate neuron firing, reduce inflammation, increase neuroplasticity, help turn glucose into energy, prevent plaque from building up and improve blood flow in the brain.” A recent review published in Brain Medicine suggests there are a “huge number of neurological diseases that can be affected by sex hormone fluctuations.”
- The Wall Street Journal reports,
- “Mounting evidence suggests that vaccination against the varicella zoster virus—which causes chickenpox in children and triggers shingles in adults—also protects the brain.
- “Several recent studies suggest that the vaccines reduce the risk of dementia in older adults, but key questions remain, including How the vaccines might work to stop or delay the condition, and whether the benefit is limited to people of a certain age.
- “The vaccines studied, Zostavax and Shingrix, both appeared to offer protection.
- “The latest study found that among 70- and 80-year-olds in Australia, people who were eligible to get the Zostavax shot were 1.8 percentage points less likely to get a dementia diagnosis in the next 7.4 years than those who were ineligible. The study was published in the journal JAMA Wednesday.”
- Per a National Cancer Institute (NCI) news release,
- “New immune-based treatments for kidney and pancreatic cancer have shown promising results in two small clinical trials. In both trials, the treatments appeared to prevent cancer from returning in patients who had successful surgery to remove their tumors.
- “The treatments are called therapeutic cancer vaccines because they help the immune system eliminate an existing cancer.
- “In both trials, the treatments were made specifically for each patient based on intensive genetic analyses of their tumor samples collected during surgery. The analyses allowed the research teams to identify mutated proteins, known as neoantigens, on each patient’s cancer cells. These rogue proteins can act like an activated security alarm to the immune system, alerting it that the cancer cells are threats that should be killed.
- “For different reasons, however, this alarm system fails. The neoantigen-based treatments are designed to step into this breach, reinforcing to the immune system that any cells displaying these mutated proteins must be eliminated.
- “In both studies, patients received multiple doses of their personalized treatments in the months following surgery. Giving the therapy after surgery is intended to kill any remaining cancer cells elsewhere in the body and potentially establish a small band of immune cells that can recognize and kill any cancer cells that pop up in the future.”
- The NCI’s Cancer Information Highlights consider “Physical Activity | Dormant Cancer Cells | Young People with Advanced Cancer.”
- Per STAT News,
- “The young people who wanted to quit e-cigarettes didn’t necessarily think they were addicted. But they did think nicotine cravings were a problem. When they enrolled in a Massachusetts General Hospital trial, they told researchers they couldn’t study in the library or work at their desks for long before getting the urge to vape. “They really didn’t like that loss of control,” said Eden Evins, director of the Center for Addiction Medicine at Mass General.
- “Using the oral pill varenicline in combination with behavioral counseling is the most effective way for young people to get that control back, according to the results of the study co-authored by Evins, published Wednesday in the Journal of the American Medical Association. Of participants ages 16 to 25, half of those who took varenicline for 12 weeks were able to abstain from e-cigarettes for the last month of that period, compared to 14% of the placebo group. After a total of six months, 28% of people in the varenicline group were still vape-free, compared to 7% of the placebo group.”
- Per Fierce Pharma,
- “Akeso and Summit Therapeutics’ giant-killing, PD-1xVEGF bispecific antibody ivonescimab has posted another phase 3 trial win in lung cancer, this time as part of a chemotherapy combination.
- “An independent data monitoring committee has determined that the HARMONi-6 trial for the first-line treatment of advanced squamous non-small cell lung cancer (NSCLC) has met its primary endpoint of progression-free survival (PFS), Akeso said Tuesday.
- “At the first pre-specified interim analysis of the 532-patient Chinese study, ivonescimab plus chemotherapy “decisively beat” BeiGene’s PD-1 inhibitor Tevimbra plus chemotherapy, Akeso said. The results—which will be presented at a medical conference later this year—were “statistically significant and clinically meaningful,” the Chinese company added.”
- and
- “Schizophrenia drug Cobenfy, a key component in Bristol Myers Squibb’s plan to navigate a transition period of major loss of exclusivity, has hit a phase 3 setback.
- “Cobenfy as an adjunctive treatment to atypical antipsychotics failed to show superior efficacy versus placebo with atypicals when used in patients with inadequately controlled schizophrenia, according to results from the phase 3 Arise trial, Bristol Myers said Tuesday.
- “The trial logged a numerical improvement, with adjunctive Cobenfy showing a 2-point reduction compared with placebo on the primary endpoint of reduction in the Positive and Negative Syndrome Scale (PANSS) total score at week 6. However, the number didn’t reach statistical significance. PANSS is a clinician-administered tool used to assess schizophrenia symptoms.”
From the U.S. healthcare business front,
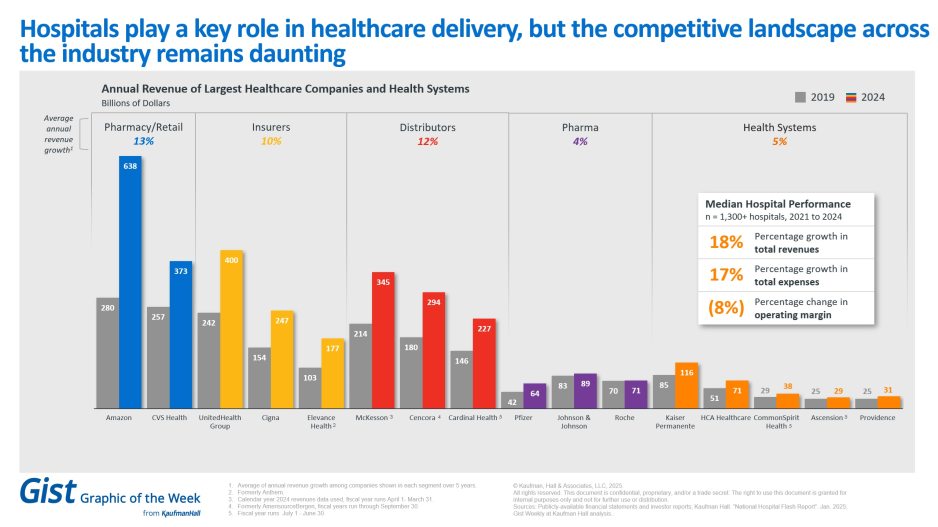
- Modern Healthcare reports,
- “Healthcare spending continues to plague employers — but most aren’t yet taking sizable steps to curb costs.
- “Nearly 85% of employers say surging healthcare prices are their biggest benefits challenge, according to a survey of about 1,800 plan sponsors nationwide published Wednesday from insurance brokerage and consulting company Lockton.
- “Employers are bracing for healthcare costs to balloon 6%-8% this year, especially as workers seek more expensive specialty care.”
- Becker Payer Issues adds,
- “There may be a link between rising insurance premiums and increased utilization of services, particularly across the Medicare Advantage space.
- “In its first quarter earnings report, UnitedHealth Group reduced its year-end earnings outlook amid rising use of physician and outpatient services among its Medicare Advantage membership and “unanticipated changes in the profile of Optum Health members.”
- “One key insight that emerged from the company was a major rise in elective care activity, which was linked directly to the higher premiums faced by some of UnitedHealth’s group MA members. The company reported that among some public sector retiree groups, premiums had increased dramatically (in some cases by as much as $150 a month) from $50 to $200. Instead of disengaging from using their benefits, these members appear to have engaged more than usual.
- “We’re seeing a significant and disproportionate increase in utilization largely within our public sector group retiree business. This population experienced the greatest year-over-year premium increases,” UnitedHealthcare CEO Tim Noel told investors. “We did assume that we would see some care activity level increases in this population, but we’re seeing far surpasses what we would have recently anticipated. And in that population as well, we are seeing more preventative care, more annual wellness visits, more in-home clinical assessments. The driver there is also really the follow-on care that results from that.”
- Fierce Healthcare relates,
- “Community Health Systems’ narrow first-quarter net loss landed right in line with Wall Street’s expectations, though the public for-profit hospital operator increased its net operating revenue on solid demand, according to financial results released Wednesday after market close.
- “Even though healthcare providers are navigating significant change as our operating environment continues to evolve, we remain confident that our strategies are strengthening our operations and positioning the company for long-term success,” CEO Tim Hingtgen said in the results announcement.
- “Net loss attributable to the company was $13 million (-$.10 per diluted share), an improvement over the $41 million loss (-$0.32) of the prior year’s first quarter—though the losses were narrower for both periods after adjustments (for impairment and loss on sale of business and related costs).
- “Net operating revenues landed at $3.16 billion, just above expectations and a 0.6% year-over-year increase. On a same-store basis taking CHS’ recent divestitures into account, net operating revenues rose by 3.1%. Both of those came alongside a 1% decrease in total admissions and a 2.3% dip in adjusted admissions, but respective same store increases of 4% and 2.6%.”
- MedTech Dive notes,
- “Boston Scientific CEO Mike Mahoney told investors Wednesday the company expects an impact of about $200 million this year due to the Trump administration’s tariff policies, becoming the latest medtech company to forecast an impact of hundreds of millions of dollars.
- “However, Boston Scientific, like others that have reported, still expects to perform well in 2025. Mahoney said Boston Scientific is “very bullish” on the year, and the firm raised its 2025 guidance from a growth range of 12.5%-14.5% on a reported basis to 15%-17%, even with the $200 million charge.”
- Per KFF,
- “The growing role of Medicare Advantage has been a defining feature of Medicare in recent years, with Medicare Advantage plans now covering more than half of all eligible Medicare beneficiaries. While most Medicare Advantage enrollees (and most people with Medicare overall) live in urban areas, as of 2024, most Medicare beneficiaries who live in the nation’s most rural counties are enrolled in traditional Medicare, not Medicare Advantage. This means that reliance on Medicare’s stand-alone prescription drug plans (PDPs) for coverage of the Medicare Part D prescription drug benefit is likely to be greater among Medicare beneficiaries living in the most rural parts of the country.”
- “The growing role of Medicare Advantage has been a defining feature of Medicare in recent years, with Medicare Advantage plans now covering more than half of all eligible Medicare beneficiaries. While most Medicare Advantage enrollees (and most people with Medicare overall) live in urban areas, as of 2024, most Medicare beneficiaries who live in the nation’s most rural counties are enrolled in traditional Medicare, not Medicare Advantage. This means that reliance on Medicare’s stand-alone prescription drug plans (PDPs) for coverage of the Medicare Part D prescription drug benefit is likely to be greater among Medicare beneficiaries living in the most rural parts of the country.”
- MedPage Today lets us know,
- “Novavax’s closely watched COVID-19 vaccine is on track for full approval after additional discussions with the FDA, the company said Wednesday.
- “The news sent company shares soaring more than 21% in morning trading and appeared to resolve concerns that Trump administration officials might be holding up a decision on the shot.
- “Novavax makes the nation’s only traditional protein-based COVID-19 vaccine. It is still being sold under emergency use authorization — unlike mRNA vaccines made by Pfizer and Moderna that have earned full FDA approval for certain age groups.”