Midweek update
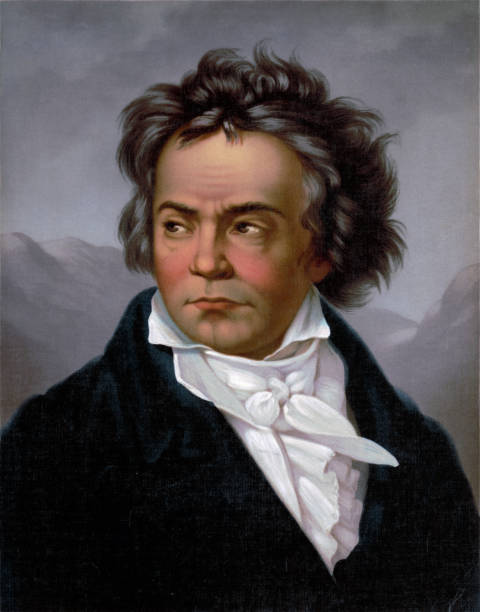
It’s the 250th anniversary of the birth of that great composer Ludwig van Beethoven. Speaking of birthdays, the FEHBlog heard today that Dr. Anthony Fauci turns 80 on December 24. According to the Washington Post, he is urging Americans to have a merry little Christmas. Touche.
On the omnibus/COVID-19 relief bill front, Bloomberg reports that
Congressional leaders are still haggling over the final details of nearly $900 billion in coronavirus aid as staff members try to write the legislative language needed for House and Senate votes this week.
If the aid deal, combined with a spending bill needed to fund the government, isn’t ready to get a vote in both chambers by Friday, another stopgap measure will be needed to avert a partial government shutdown after midnight Friday.
People briefed on the negotiations say the draft of the plan includes $600 in payments for individuals, $300-per-week in supplemental unemployment insurance payments and aid for small businesses, but it omits aid to state and local governments and lawsuit liability protection. It also includes roughly $17 billion for airlines.
Senate Majority Leader Mitch McConnell, House Speaker Nancy Pelosi, Senate Democratic leader Chuck Schumer and House Republican leader Kevin McCarthy continued negotiations on Wednesday, although the deal is more likely to come together by Thursday, according to a lawmaker briefed on the talks.
The FEHBlog expected the legislative language today but good things come to those who wait, right?
The CMS actuary released his annual report on the previous year’s healthcare spending. “Total national healthcare spending in 2019 grew 4.6%, which was similar to the 4.7% growth in 2018 and the average annual growth since 2016 of 4.5%.” 2020 may be the outlier.
Healthcare Dive reports that
HHS began distributing the third phase of COVID-19 relief funding for providers Wednesday, with $24.5 billion to go to more than 70,000 providers through the end of January. The amount exceeds the original $20 billion planned for this tranche as officials realized more would be needed to get providers close to whole from coronavirus-related losses. HHS said up to 88% of applicants’ reported losses are being reimbursed.
In that regard, Fierce Healthcare reports that major healthcare systems which own a health insurer are weathering the COVID-19 storm better than most health systems according to a PwC report. “PwC pointed to major health systems such as Intermountain, Kaiser Permanente and Presbyterian Healthcare Services that used health plans to help bolster their finances.” It’s not surprising to the FEHBlog that hedges like this work. Large health insurers similarly are acquiring healthcare providers.
In other news —
- The EEOC offers guidance for employers who want to make sure that their employee are vaccinated again COVID-19 and also want to comply with federal anti-discrimination law. This new guidance is Q&A K.
- EHR Intelligence discusses the Gravity Project’s efforts to introduce social determinants of health data into electronic health records.
- Health Payer Intelligence informs us about a PwC Health Research Institute report concluding that “Payers and stakeholder collaborators have the opportunity to rebuild the healthcare system into a more effective and consumer-centric system in 2021 by honing virtual care and other strategies.”
- Krebs on Security details the malicious hack on the SolarWinds/Orion platform used by federal agencies and Fortune 500 companies “to monitor the health of their IT networks.”











