Tuesday’s Tidbits

The Centers for Medicare and Medicaid Services (CMS) announced its proposed national coverage decision for Biogen’s Alzheimers Disease FDA-approved treatment, Aduhelm, today.
The proposed National Coverage Determination would cover Food and Drug Administration (FDA) approved monoclonal antibodies that target amyloid for the treatment of Alzheimer’s disease through coverage with evidence development (CED) – which means that FDA-approved drugs in this class would be covered for people with Medicare only if they are enrolled in qualifying clinical trials. The proposed National Coverage Determination is open to public comment for 30 days.
STAT News sums it up as follows:
Normally, Medicare covers drugs if the FDA approves them. Aduhelm has been different because the agency approved the treatment without a guarantee that patients actually will see slower cognitive decline. The process that led to the drug’s approval is the subject of multiple investigations, following STAT’s reporting that Biogen had an extensive back-channel relationship with the FDA. * * *
Medicare officials don’t require participation in clinical studies for beneficiaries very often — there are only about two dozen other health care products with a similar designation, called a Coverage with Evidence Development (CED), listed on Medicare’s website. Most are for medical devices or diagnostic imaging, and are less restrictive than the policy Medicare announced Tuesday. * * *
Sean Tunis, a principal at Rubix Health who helped develop the CED process during his tenure at the Centers for Medicare and Medicaid Services, said the proposal is almost as restrictive as if Medicare had decided not to cover the drug at all. Medicare, he estimated, would pay for drug costs for perhaps a few thousand patients that enroll in randomized trials over the next three to five years.
The CMS national coverage decision if finalized would help the FEHB Program dodge a bullet because it has many annuitant enrollees without Medicare Part B and for whom the FEHB plan would be the primary Aduhelm payer.
Following up on yesterday’s post about Affordable Care Act FAQ 51 implementing the President’s mandate on health plans to cover over the counter COVID tests, the FEHBlog noticed the fourth FAQ in this section of FAQ 51 which reads as follows:
Q4: When providing coverage of OTC COVID-19 tests, are plans and issuers permitted to address suspected fraud and abuse?
Yes. As stated in FAQs Part 44, Q2, although the FFCRA prohibits medical management of coverage of COVID-19 diagnostic testing, plans and issuers may act to prevent, detect, and address fraud and abuse. Examples of permissible activities include the following:
- A plan or issuer may take reasonable steps to ensure that an OTC COVID-19 test for which a covered individual seeks coverage under the plan or coverage was purchased for the individual’s own personal use (or use by another participant, beneficiary, or enrollee who is covered under the plan or coverage as a member of the individual’s family), provided that such steps do not create significant barriers for participants, beneficiaries, and enrollees to obtain these tests. For example, a plan or issuer could require an attestation, such as a signature on a brief attestation document, that the OTC COVID-19 test was purchased by the participant, beneficiary, or enrollee for personal use, not for employment purposes, has not been (and will not be) reimbursed by another source, and is not for resale. In contrast, the Departments are of the view that fraud and abuse programs that require an individual to submit multiple documents or involve numerous steps that unduly delay a participant’s, beneficiary’s, or enrollee’s access to, or reimbursement for, OTC COVID-19 tests are not reasonable.
- A plan or issuer may require reasonable documentation of proof of purchase with a claim for reimbursement for the cost of an OTC COVID-19 test. Examples of such documentation could include the UPC code for the OTC COVID-19 test to verify that the item is one for which coverage is required under section 6001 of FFCRA, and/or a receipt from the seller of the test, documenting the date of purchase and the price of the OTC COVID-19 test.
It occurred to the FEHBlog that FSAFeds the flexible spending account program for federal employees must be reimbursing participants for OTC Covid test kits. In fact the FSAFeds does offer reimbursement for OTC test kits on the condition that the participant furnishes a detailed receipt. For OTC products, FSAFeds generally requires a receipt including Vendor name, Date of purchase, Product name, and Cost. This should be a reasonable documentation standard for FEHB plans to adopt.
Also from the testing front, the Wall Street Journal looks into the reliability of rapid antigen COVID tests sold OTC.
Rapid antigen tests are a useful tool if we are smart about how we use them.
Because the data suggest that rapid tests may be yielding more false negatives at the beginning of an Omicron infection, you’ll have a better chance of getting an accurate result if you wait a day or two after developing symptoms to test, says Katelyn Jetelina, assistant professor of epidemiology at the University of Texas Health Science Center at Houston. If your test is negative, take a second test a day or two later, or get a PCR test if you can. (Easier said than done these days.)
Understand the limitations of rapid tests if you’re considering using them to screen people before gatherings. Rapid tests before a wedding or other large indoor gathering could miss early infections that could be contagious, Dr. [Blythe] Adamson says.
If you have a positive rapid test, you almost definitely have Covid-19, Dr. [Gigi] Gronvall says. False positives are rare, especially when case rates are as high as they are now. You likely don’t need to confirm a positive rapid-test result with a follow-up PCR test, unless an employer or other institution requires it.
In other Omicron news —
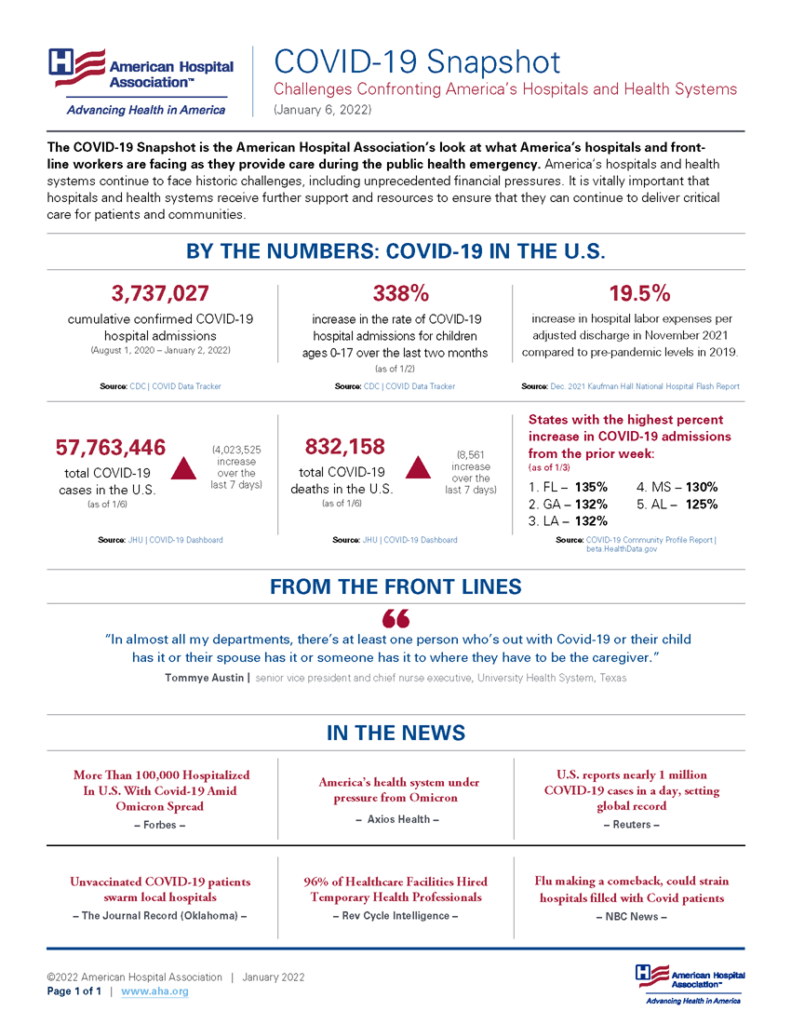
- The Wall Street Journal reports that “U.S. hospitals are caring for the highest number of patients with Covid-19 reported during the pandemic, according to federal government data, as the Omicron variant worsens pressures on the already strained facilities.”
- The Journal also tells us that “U.S. officials on Tuesday ordered 600,000 doses of Covid-19 treatment sotrovimab, the only monoclonal antibody therapy thought to work against the Omicron variant, as a record number of cases puts hospitals under increasing pressure in parts of the U.S. and Europe. Sotrovimab, made by GlaxoSmithKline PLC and Vir Biotechnology Inc., is now the only Covid-19 monoclonal antibody available for patients in the U.S.”
ACA FAQ 51 also includes reminders to health plans about the wide scope of the ACA’s contraceptive mandate.
From the federal employee COVID vaccination front Federal News Network reports that
The first update by the Safer Federal Workforce task force in more than a month is addressing the challenge of testing employees and contractors who work on-site or with the public on a regular basis for COVID-19, the types of tests that are permitted and who is responsible for paying for said tests.
The crux of the updated and new frequently ask questions is agencies have until Feb. 15 to set up a testing program “for employees who are not fully vaccinated, including due to a pending or approved request for exception or extension from the COVID-19 vaccination requirement for federal employees.”
The task force said the testing program is only for employees who work on-site or interact with the public like safety inspectors, and not for those who work remotely.
Fedweek adds that “A period of waiting is continuing on two major federal workplace issues on which action was expected around now—enforcement of the Coronavirus vaccine mandate and the “reentry” from telework to regular worksites by more employees and for more often.”
From the preventive services department, the Department of Health and Human Services announced today that
Today, the U.S. Department of Health & Human Services (HHS) announced that the Health Resources and Services Administration (HRSA) has updated comprehensive preventive care and screening guidelines for women and for infants, children, and adolescents. Under the Affordable Care Act (ACA), certain group health plans and insurance issuers must provide coverage with no out-of-pocket cost for preventive health services within these HRSA-supported comprehensive guidelines. Among a number of updates, for the first time the guidelines will require such group health plans and insurance plans to provide coverage without a co-pay or deductible for double electric breast pumps.
Fierce Healthcare reports news from the second day of the JPMorgan Healthcare Conference.
From the tidbits department —
- Last week, the Office of National Coordinator for Health Information Technology announced “the release of the Project US@ (“Project USA”) Technical Specification Final Version 1.0 and thereby completed our one year goal to coordinate the creation of a health care specification that could be used across the industry for representing patient addresses (mailing, physical, billing, etc.). This new “tech spec” will advance the health care industry’s proficiency in recording and managing accurate and consistently formatted patient addresses and support more efficient patient matching and record linkage. As a reminder, among the many data elements that are used in patient matching, research has shown patient address to be one of the most sensitive to standardization and therefore impactful on patient matching, especially at scale. However, patient addresses change frequently, are often entered incorrectly or imprecisely.”