Tuesday Tidbits

Happy Ides of March. The President signed the Consolidated Appropriations Act 2022 into law today. The Postal Reform Act of 2022 continues to await the President’s signature.
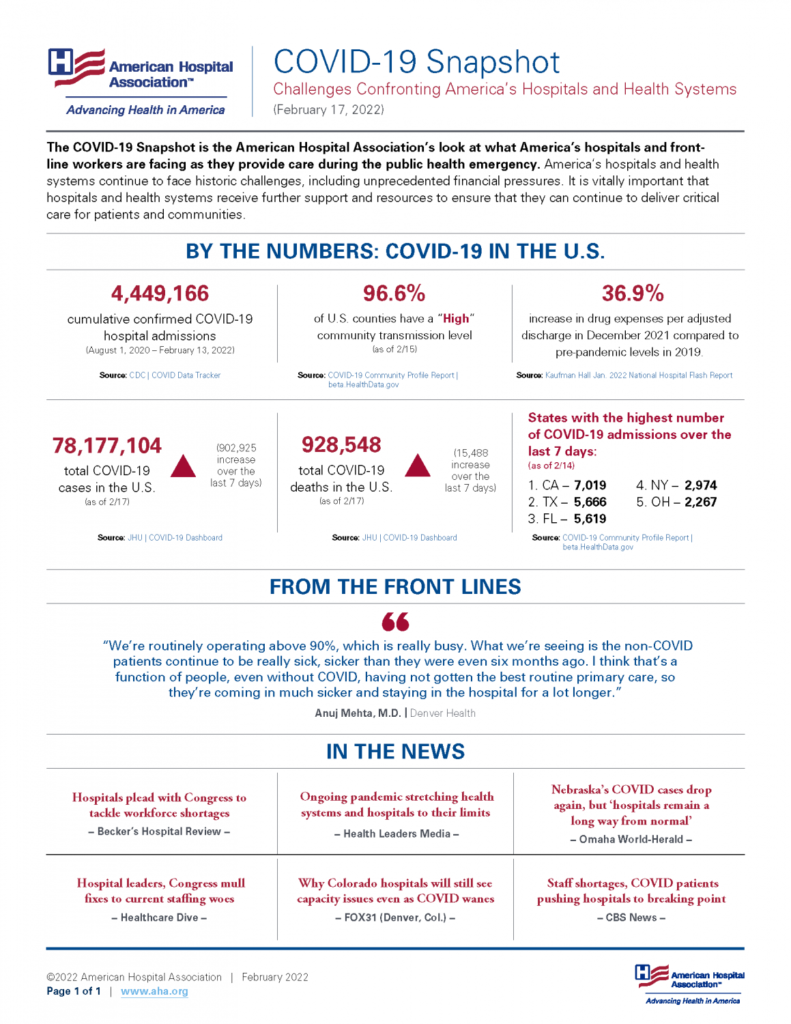
From the Omicron front, David Leonhardt reports on COVID surges in China and Europe. He concludes
Even if [Covid] cases rise [in the U.S. again], as seems likely, there are good reasons not to panic. Vaccination tends to turn Covid into a mild illness, especially for people who have received a booster. For the unvaccinated and unboosted, BA.2 is another reason to get a shot.
It’s also a reason for the federal government and states to expand access to both Evusheld — a drug that can help protect the immunocompromised — and Paxlovid — a post-infection treatment. Finding either is often difficult today. (If you’re looking for one of them, click on this link for Evusheld and this one for Paxlovid.)
The bottom line: Covid isn’t going away, but vaccination and other treatments can keep future increases manageable. The biggest problem remains the millions of people who remain unvaccinated, many of them by choice. That’s the case in the U.S., in Hong Kong and across much of Europe, Africa and the rest of the world.
Inducing more people to get shots — through persuasion or mandates — would probably save more lives than any other Covid policy.
What is the FDA’s hold up in reviewing the standard Covid vaccines for which emergency use authorizations have been filed? As previously noted, the traditional vaccines may be appealing to those resistant to the state-of-the-art mRNA vaccines.
The Wall Street Journal reports
Pfizer Inc. and partner BioNTech SE have asked U.S. health regulators to authorize a second booster dose of its Covid-19 vaccine for people 65 years and older.
The companies said Tuesday that they had filed the application. The Food and Drug Administration is expected to make a decision in time for the Biden administration to begin a potential fall vaccine campaign.
The FDA has been reviewing data and looking at potentially authorizing a fourth dose of the shot for use in the fall, The Wall Street Journal reported last month.
From the Rx coverage front —
STAT News informs us
The prices pharmacy benefit managers and insurers pay for Sanofi medicines have decreased for a sixth consecutive year, yet patient out-of-pocket costs are rising. Once again, there is further evidence that focusing solely on lowering the list price of medicines doesn’t guarantee lower costs for patients. Sanofi pulls back the curtain on the impact of list and net prices and more in its annual pricing report.
and
Back in 2019, when the Senate Finance Committee called seven drug industry CEOs to testify, it seemed like proof that Washington was within striking distance of actually reining in the industry’s high prices. “It’s past time to get beyond the excuses and make prescription drugs affordable,” Sen. Ron Wyden, the top Democrat on the committee, told drugmakers that day. Tomorrow, almost exactly three years later, Wyden will chair another hearing on prescription drug pricing. He’s billing the hearing as “an opportunity for members to discuss how high drug prices have impacted seniors and families in their states and identify solutions” — even though lawmakers have had more than a dozen such hearings to “discuss” high drug prices over the past three years. STAT’s Nicholas Florko tallies what’s at stake in STAT+.
In FDA News, the agency reports approving today “the first generic of Symbicort (budesonide and formoterol fumarate dihydrate) Inhalation Aerosol for the treatment of two common pulmonary health conditions: asthma in patients six years of age and older; and the maintenance treatment of airflow obstruction and reducing exacerbations for patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and/or emphysema. This complex generic drug-device combination product, which is a metered-dose inhaler, should not be used to treat acute asthma attacks.”
From the opioid epidemic front, “the Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA), announced two grant programs totaling $25.6 million that will expand access to medication-assisted treatment for opioid use disorder and prevent the misuse of prescription drugs. By reducing barriers to accessing the most effective, evidence-based treatments, this funding reflects the priorities of HHS’ Overdose Prevention Strategy, as well as its new initiative to strengthen the nation’s mental health and crisis care systems.”
From the patient front, HHS’s Agency for Healthcare Research and Quality announced the agency’s
Support for Patient Safety Awareness Week. Ongoing investments in safety research, the development of safety toolkits and training resources, and a growing emphasis on improving diagnostic safety are all part of a mission to make healthcare safe for all Americans. Access more information about AHRQ’s support of Patient Safety Awareness Week, including a special introductory video from Jeff Brady, M.D., director of the Center for Quality Improvement and Patient Safety; information about how to get involved in Patient Safety Awareness Week activities; and recent patient and diagnostic safety resources, including:
— Safer Together: A National Action Plan to Advance Patient Safety
— Making Healthcare Safer III: A Critical Analysis of Existing and Emerging Patient Safety Practices
— AHRQ QuestionBuilder App (also available in Spanish)
From the HIMSS conference in Orlando, Healthcare Dive tells us
The Biden administration has been working on additional rulemaking to address issues with the payer-to-payer data exchange requirements set out in sweeping interoperability rules finalized in early 2020, and “we look forward to sharing this rule with you soon,” CMS administrator Chiquita Brooks-LaSure told attendees at the HIMSS annual conference in Orlando on Tuesday.
CMS decided not to enforce those provisions when they kicked in this year, after health insurers raised concerns about operational challenges and risks to data quality given a lack of specificity in the rule.
The new rule will incorporate extensive public comment to try to address stakeholder concerns, and will standardize how payers exchange data through application programming interfaces, Brooks-LaSure said.
An online tool that allows patients in markets across the country to compare prices for hundreds of hospital services before getting treatment has launched in its beta development stage.
Turquoise Health’s platform uses cost data from machine-readable files made public by hospitals as part of compliance with a federal price transparency rule that went into effect in January 2021.
The San Diego-based startup’s platform includes a scorecard that lets users assess price transparency compliance with the CMS requirements for nearly 6,000 hospitals, Turquoise Health said Monday. Hospitals receive a score based on an algorithm-driven five-star rating system.
Fierce Healthcare reports from the SXSW Conference in Austin, TX.
Samsung and Best Buy executives shared why they place big bets on tech to help elderly Americans age at home.
Experts are laying out the business case to invest in care for underserved communities.
Leaders in women’s health say empowering female patients is key to addressing gender biases in healthcare.