Monday Roundup

Tonight the House is voting on the Consolidated Appropriations Act, 2021(Amendment to H.R. 133), which includes the Fiscal Year 2021 omnibus spending bill, COVID-19 relief measures, and a whole lot more. After the House votes, the Senate will vote and send the Congressionally approved bill along to the President for his expected signature.
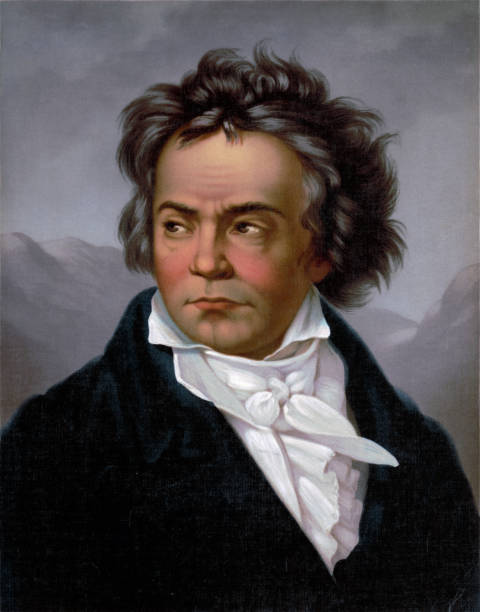
Late this afternoon, the FEHBlog found, thanks to the Hill, a complete version of the bill which included 400 pages of complicated amendments to the Affordable Care Act (Division BB). However, when the FEHBlog tried to find that version on the House Rules Committee website tonight in connection with this post, he couldn’t. There’s no sense delving into those healthcare provisions until a law is passed. In the words of John Godfrey Saxe (according to WikiQuotes), “Laws, like sausages, cease to inspire respect in proportion as we know how they are made.”
(P.S. This morning Bloomberg reports that Congress passed H.R. 133 by wide margins. Congress wisely also passed a seven day extension of the current continuing resolution funding the federal government because as Bloomberg reports)
Before the president can sign the full package, it must be enrolled on parchment paper, physically delivered to the White House and reviewed by administration lawyers — a process complicated by the pandemic and coming Christmas holiday.)
Moving on, under current law, a prescription drug manufacturer cannot sell a prescription drug at a price below the best price paid by Medicaid. Only Medicare Part D is excepted from that rule. Today, the Centers for Medicare and Medicare Services (“CMS”) finalized a rule that creates a second exception for value based pricing arrangement. CMS explains:
Under current regulations, prescription drug manufacturers face challenges accounting for VBP arrangements in their Medicaid best price reporting to CMS. This has the unintended consequence of hindering providers, insurers and prescription drug manufacturers in their efforts to develop innovative payment models for new drug therapies and other innovative treatments. Current regulations also discourage payers and manufacturers from designing new payment arrangements based on the value their product may provide.
With the new flexibilities under this final rule, manufacturers will be more willing to negotiate with payers, including Medicaid, with drug pricing being driven by the value of their drug to the individual patient. This is significant, especially in the era of new genetic-based treatments which may initially be expensive, yet in the long run offer significant value to the patient and payer. Payers will be able to negotiate prices with manufacturers for these genetic-based treatments based upon outcomes and evidence-based measures such as reduced hospitalizations, lab visits, and physician office visits, ensuring that if such measures fail to support the value of a drug, the payer is not held accountable for the full price.
Today’s final rule codifies a broad definition of VBP, which can better align pricing and payment to observed or expected evidence and/or outcomes-based measures in a targeted population. The final rule also allows manufacturers to report multiple best prices instead of a single best price when offering their VBP arrangements to all states. By making these changes, effective in January 2022, CMS hopes to encourage VBP arrangements and negotiations to help make new, innovative therapies more available to all patients. As a result, it is estimated that these new VBP approaches could save up to $228 million in Federal and state dollars through the year 2025.
Bravo. This action will support FEHB plan efforts to control drug costs.
On the Solarwinds backdoor hack front, Federal News Network discusses its impact on federal government cybersecurity efforts.