Thursday Miscellany

From Capitol Hill, the Senate has adjourned until Monday March 7 after setting another cloture vote on the Postal Reform Act of 2022 (HR 3076) for Monday at 5:30 pm. While the FEHBlog is not a Senate procedure expert, it appears that another cloture vote is required because a minor Senate amendment was filed after the first cloture vote. Postal reform must be getting real because the Wall Street Journal posted an account of the decade-long effort to pass this legislation today.
From the Omicron front, the FEHBlog’s favorite part of the President’s new strategy was explained by the White House Covid czar yesterday:
Pfizer’s pill {Paxlovid] is a gamechanger — 90 percent effective at keeping people out of the hospital.
We collaborated with Pfizer to accelerate development of the pill. And we’ve ordered 20 million courses.
As the President announced last night, Pfizer worked overtime to further accelerate delivery. This month alone — the month of March — we’ll have 1 million of these treatment courses available. And in April, that number will more than double.
To ensure these lifesaving treatments are easily accessible, the President’s Plan launches a new “Test to Treat” initiative to provide individuals access to testing and treatment for free, all in one stop.
Hundreds of one-stop sites will open across the country this month, located at local pharmacy clinics, community health centers, long-term care facilities, and veterans’ health centers.
Marketwatch adds today that “CVS Health Corp., the Walgreens Boots Alliance Inc., and Walmart Inc. said they will participate in the test-to-treat initiative, a new program that allows someone who has tested positive for the virus to get antiviral pills during the same visit at no cost.”
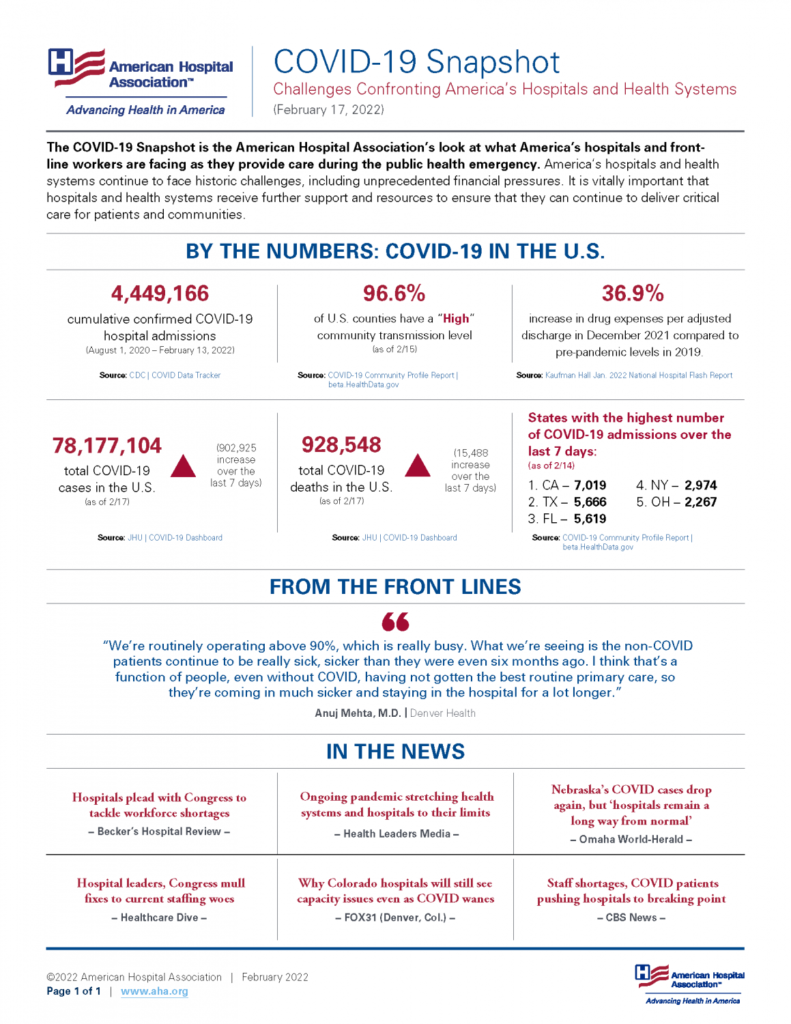
Covid treatment costs were astronomical because care principally was given in hospitals and other healthcare facilities, creating a major burden on the healthcare system. Facilitating the use of Flonase for Covid will avoid the vast majority of those hospitalizations, thereby lowering healthcare costs.
Speaking of testing, the Wall Street Journal reports that
Manufacturers are developing new types of at-home tests, including for flu and strep throat, aimed at consumers who are increasingly monitoring and managing their own health through fitness apps and smartwatches.
Boulder, Colo.-based fertility company MFB Fertility Inc. received clearance from the U.S. Food and Drug Administration in February 2020 for its Proov test, designed to help women measure their hormone levels and to know when in a given month they are most likely to become pregnant. A typical kit includes 20 testing strips, allowing a woman to test daily, which the company said would be tough to achieve through visits to a doctor’s office.
Amy Beckley, the company’s chief executive, said the rise of at-home Covid-19 tests over the past year has made it much easier for people to understand her product.
“All of a sudden, home diagnostics and home testing became a thing,” she said.
Mobihealth News reported last June
The U.S. Air Force has inked a $1.3 million deal with MFB Fertility in order to provide military members and their partners the former’s home fertility tests.
The Air Force’s AFWERX office will invest in Proov, an at-home ovulation test with FDA clearance. The test works by measuring Pregnanediol Glucuronide (PdG), the urine metabolite of progesterone, which is released by the ovary after ovulation. High levels of PdG over multiple days can confirm that successful ovulation took place.
The contract will provide free Proov kits to Air Force couples upon request and connect them to fertility specialists.
Two cool innovations.
From the healthcare policy front —
- The White House released a fact sheet on steps underway to address the Nation’s opioid epidemic.
- The Associated Press reports on the President’s mental healthcare policy proposals made in Tuesday’s State of the Union address. For example, under the President’s plan, “Health insurance plans would have to cover three mental health visits a year at no added cost to patients.” I suggest that the Administration consider the fact that most employers offer employee assistance plans that already offer two or three free mental health therapy visits. The overcomplicated federal mental health parity law fails to look at the big picture.
From the diabetes front —
- The AMA offers six tips for screening patients for pre-diabetes. Many of the tips also could be applied by health plan case managers and coaches.
- The American Diabetes Association delves into the relationship between diabetes and kidney disease.
From the litigation front, Reuters reports
The Sackler family owners of Purdue Pharma LP reached a deal with a group of attorneys general to pay up to $6 billion in cash to resolve widespread litigation alleging that they fueled the U.S. opioid epidemic, bringing the OxyContin maker closer to exiting bankruptcy.
The attorneys general for eight states and the District of Columbia, who had blocked a previous settlement that included a $4.3 billion cash payment, announced the deal after weeks of mediation with the Sacklers.
The family agreed to pay at least $5.5 billion in cash, which will be used for abating a crisis that has led to nearly 500,000 U.S. opioid overdose deaths over two decades.
The value of the deal could grow as the family members sell additional assets.
U.S. Bankruptcy Judge Robert Drain must approve the deal, which protects the Sacklers from civil lawsuits. Purdue requested a March 9 hearing for Drain to review the agreement.
From the Rx coverage front, Biopharma Dive reports
Civica is making plans to offer three versions of insulin that can be sold at dramatically lower prices than today’s alternatives, targeting a need highlighted by President Joe Biden during this week’s State of the Union Address.
The nonprofit company, created by hospital systems and philanthropies to address drug shortages, said Wednesday it will recommend pricing of no more than $30 for the vials it produces. Name-brand versions can currently cost 10 times that amount at cash prices.
Civica announced an ambitious timeline, projecting that the first product — designed to be interchangeable with Sanofi’s Lantus — would be available as soon as early 2024. The company also aims to manufacture cheaper versions of Eli Lilly’s Humalog and Novo Nordisk’s Novolog, in both vials and pre-filled pens.
Also the Institute for Clinical and Economic Review (“ICER”) announced
it will assess the comparative clinical effectiveness and value of subcutaneous semaglutide (Wegovy, Novo Nordisk), phentermine / topiramate (Qsymia, Vivus Pharmaceuticals), liraglutide (Saxenda, Novo Nordisk), and naltrexone/bupropion (Contrave, Currax Pharma) for the treatment of obesity.
The assessment will be publicly discussed during a meeting of the New England Comparative Effectiveness Public Advisory Council (New England CEPAC) in September 2022, where the independent evidence review panel will deliberate and vote on evidence presented in ICER’s report.
ICER’s website provides timelines of key posting dates and public comment periods for this assessment.