Monday Roundup

Bloomberg has released its latest COVID-19 resilience ranking.
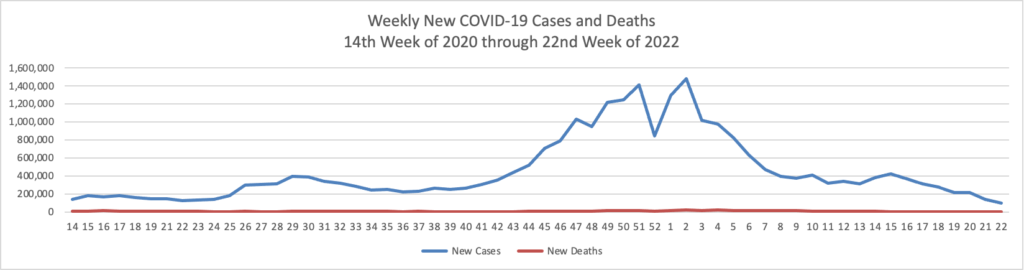
Almost a year and a half into the pandemic, the best and worst places to be in the Covid-19 era are increasingly defined by one thing: normalization.
The biggest vaccination drive in history is enabling parts of the globe to abolish mask mandates, relax restrictions and dismantle border curbs, making the magnitude of reopening key to quality of life. Taming cases and deaths was once paramount, along with ensuring a robust health-care system. Now, the ability to essentially turn back the clock and return to pre-pandemic times is taking on an even greater significance.
Central to that is an economy’s openness to the world, and that’s why we’ve introduced a new element—Reopening Progress—to Bloomberg’s Covid Resilience Ranking. Two new metrics capture the ease of moving in and out of a place and how much air travel has recovered, alongside our 10 other measures tracking mortality rates to infection counts, freedom of movement to economic growth.
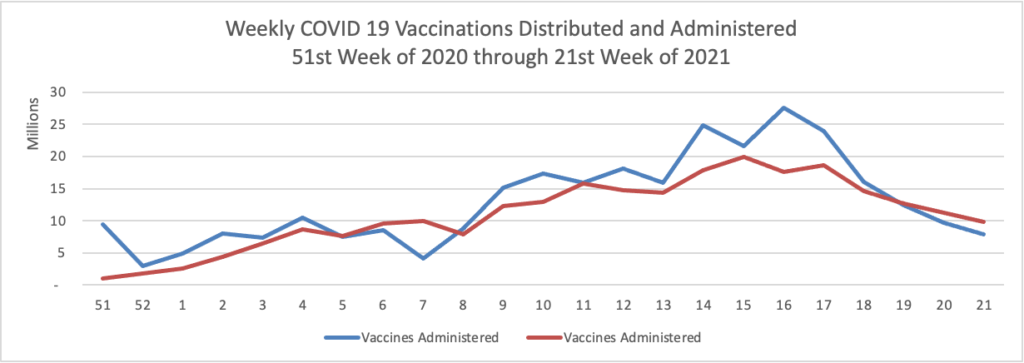
This pivot has ushered in dramatic changes to the ranks. The U.S. is now No. 1, with its fast and expansive vaccine rollout, dominated by the highly effective Messenger RNA shots, stemming what was once the world’s worst outbreak.
The U.S. Supreme Court today according to Fierce Healthcare
declined to hear an appeal of a lower court decision upholding the Department of Health and Human Services’ (HHS’) site-neutral payments policy.
The appeal was requested by the American Hospital Association (AHA) in February as part of a multiyear legal battle challenging HHS’ authority to bring Medicare payments to off-campus clinics in line with independent physician practices. The AHA’s bid was supported by a long list of other provider industry stakeholders.
By taking a pass on the case, the top court has now paved the way for HHS to move forward with the 2019 Outpatient Prospective Payment System rule—a policy the agency has said would have saved the Centers for Medicare & Medicaid Services roughly $800 million in payments to outpatient departments during 2020. * * *
HHS’ rule aims to remove payment disparities where hospital-affiliated clinics receive more Medicare reimbursement than physicians’ offices providing the same services. Researchers have suggested over the years that these disparities have played a part in provider consolidation.
Also today the Department of Health and Human Services released a third notice of Affordable Care Act Benefit and Payment Parameters as a proposed rule. Fierce Healthcare informs us that the proposed rule would set the ACA’s open season at an expanded November 1 through January 15 and also would allow exchanges to offer special enrollment periods for low income customers who may benefit from the American Rescue Plan’s expanded premium credits. Health Payer Intelligence discusses two impacts from the current ongoing special ACA open enrollment period which runs until August 15.
In other round up items
- The ICD-10 Monitor tells us that the Centers for Disease Control released new ICD-10-CM codes for federal fiscal year 2022 which include 19 new social determinants of health codes in the “Z” chapter. Many of these new “Z” codes are attributable to the Gravity Project which is an HL7 FHIR accelerator organization.
- The Wall Street Journal discusses what doctors want their patients to know about the new Alzheimer’s disease drug Aduhelm. For example, “The treatment would work over years, not weeks or months. Dr. [Paul] Aisen estimates that patients with mild cognitive impairment, which is often a precursor to dementia, might get an extra year or two before they start losing their ability to function independently.”
- Fierce Healthcare reports that
Future demand for healthcare services will be relatively flat to declining, with little to no effect from the COVID-19 pandemic, according to a new forecast report.
At the same time, hospitals and health systems are facing increasing competition from consumer businesses such as Amazon and Walmart, retail behemoths that are rapidly expanding the supply of healthcare services.
The implications of softening demand and increasing supply suggest that pricing trends are ultimately unsustainable for healthcare providers, according to a new report from health system analytics company Trilliant Health.
The company’s analysis, based on 70 billion medical claims across 309 million patient visits, contradicts the commonly held belief that the demand for healthcare services nationwide is rising, according to Sanjula Jain, Ph.D., senior vice president of market strategy and chief research officer at Trilliant Health.
Time will tell.