
Based on the Centers for Disease Control’s Covid Data Tracker, the CDC’s weekly interpretation of those new cases, hospitalizations and death statistics shows across-the-board increases. Welcome winter.
New Cases
As of December 7, 2022, the current 7-day average of weekly new cases (65,569) increased 49.6% compared with the previous 7-day average (43,825). A total of 99,241,649 COVID-19 cases have been reported in the United States as of December 7, 2022.
Variant Proportions
CDC Nowcast projections* for the week ending December 10, 2022, estimate the proportion of lineages designated as Omicron with estimates above 1%: BA.5—and four of its sublineages (BQ.1, BQ.1.1, BF.7, and BA.5.2.6)—BA.4.6, and XBB. XBB is a recombinant of two BA.2 sublineages.
The two predominant Omicron lineages and the two that are increasing this week are BQ.1.1, projected to be 36.8% (95% PI 34.1-39.6%) and BQ.1, projected to be 31.1% (95% PI 29.0-33.4%) nationally. All other lineages (BA.5, BF.7, XBB, BN.1, BA.5.2.6, and BA.4.6) are decreasing in proportion this week compared to last.
New Hospitalizations
The current 7-day daily average for November 30–December 6, 2022, was 4,844. This is a 13.8% increase from the prior 7-day average (4,256) from November 23–29, 2022.
New Deaths
The current 7-day average of new deaths (426) increased 61.7% compared with the previous 7-day average (263). As of December 7, 2022, a total of 1,080,472 COVID-19 deaths have been reported in the United States.
CNN adds,
Hospitals are more full than they’ve been throughout the Covid-19 pandemic, according to a CNN analysis of data from the US Department of Health and Human Services. But as respiratory virus season surges across the US, it’s much more than Covid that’s filling beds this year.
More than 80% of hospital beds are in use nationwide, jumping 8 percentage points in the past two weeks.
Hospitals have been more than 70% full for the vast majority of that time. But they’ve been 80% full at only one other point: in January, during the height of the Omicron surge in the US. Back in January, about a quarter of hospital beds were in use for Covid-19 patients. But now, only about 6% of beds are in use for Covid-19 patients, according to the HHS data.
From the Omicron countermeasures front, the weekly interpretation tells us
As of December 7, 2022, 657.9 million vaccine doses have been administered in the United States. Overall, about 228.6 million people, or 68.9% of the total U.S. population, have completed a primary series.* More than 42.0 million people, or 13.5% of the U.S. population ages 5 years and older, have received an updated (bivalent) booster dose.
Medscape adds, “Getting at least one dose of a COVID-19 vaccine decreases the chances of having symptoms beyond 3 weeks or developing long COVID, a new analysis shows.”
The weekly interpretation usually encourages more Covid vaccinations. This week, the interpretation opens by touting the use of Paxlovid, to wit —
As we enter the holiday season, it’s important to take steps to protect yourself and others from serious illness with COVID-19, including staying up to date on COVID-19 vaccines and promptly talking to your healthcare provider about treatment options if you test positive for COVID-19.
If you have COVID-19 symptoms:
Test : Use a self-test, locate a test site, or find a Test to Treat location.
Talk: If you test positive, talk to a healthcare professional to determine if you are eligible for treatment, even if your symptoms are mild right now.
Treat: Start treatment within five days of developing symptoms.
Note to Readers: Paxlovid is not a replacement for COVID-19 vaccination. COVID-19 vaccination makes you much less likely to get very sick. Still, some vaccinated people, especially those ages 65 years or older or who have other risk factors for severe disease, may benefit from treatment if they get COVID-19. A healthcare provider will help decide which treatment, if any, is right for you.
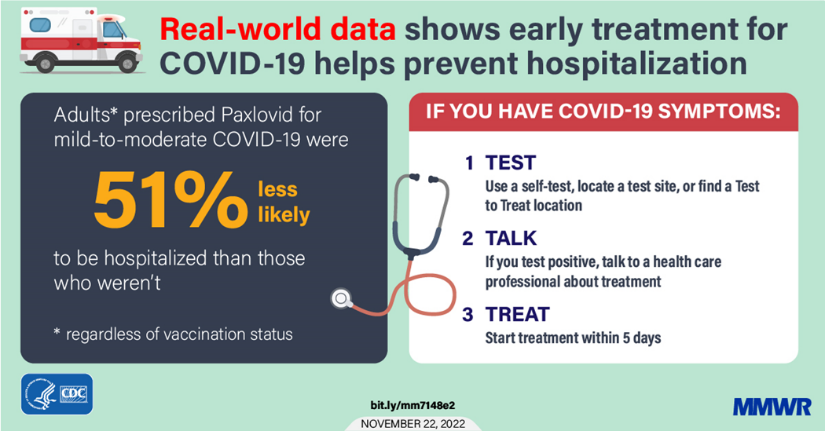
That’s the full picture for most folks. Here’s the “real-world data” link if you are interested. Thank you CDC.
Here are the key points from this week’s CDC FluView:
- Seasonal influenza activity is high across the country.
- Of the influenza A viruses detected and subtyped during week 48, 76% have been influenza A(H3N2), and 24% have been influenza A (H1N1).
- Seven influenza-associated pediatric deaths were reported this week, for a total of 21 pediatric flu deaths reported so far this season.
- CDC estimates that, so far this season, there have been at least 13 million illnesses, 120,000 hospitalizations, and 7,300 deaths from flu.
- The cumulative hospitalization rate in the FluSurv-NET system is higher than the rate observed in week 48 during every previous season since 2010-2011.
- The number of flu hospital admissions reported in the HHS Protect system increased during week 48 compared to week 47.
- The majority of influenza viruses tested are in the same genetic subclade as and antigenically similar to the influenza viruses included in this season’s influenza vaccine.
- All viruses collected and evaluated this season have been susceptible to influenza antivirals.
- An annual flu vaccine is the best way to protect against the flu. Vaccination helps prevent infection and can also prevent serious outcomes in people who get vaccinated but still get sick with the flu.
- CDC recommends that everyone ages 6 months and older get a flu vaccine annually. Now is a good time to get vaccinated if you haven’t already.
- There are also prescription flu antiviral drugs that can be used to treat flu illnesses. It’s very important that flu antiviral drugs are started as soon as possible to treat patients who are hospitalized with flu, people who are very sick with flu but who do not need to be hospitalized, and people with flu who are at higher risk of serious flu complications based on their age or health.
- Multiple respiratory viruses are currently co-circulating with influenza. Testing is important to determine the appropriate treatment.
From the FEHB front, the FEHBlog was bowled over to discover on reginfo.gov that on November 29, the Office of Personnel Management took a major step forward in implementing the Postal Service Health Benefits Program by submitting a draft interim final rule to OMB’s Office of Information and Regulatory Affairs for its review. This is the final step before the rule is published in the Federal Register. The statutory deadline for so promulgating this rule is April 8, 2023.
From the miscellany department
- HR Dive discusses a Mercer report on how employers can impact the maternal mortality problem.
- EBRI offers a useful analysis of telemedicine and its relationship with other healthcare services, enrollee health, and costs.
- Chain Drug News reports that PCMA, the prescription drug manager trade association, has issued policy recommendations to accelerate patient biosimilar drug use.
- The Wall Street Journal offers encouraging news about prison programs to resolve inmate addiction issues.
Two-thirds of people entering prisons and jails have what the Department of Health and Human Services diagnoses as substance-use disorder. For years, the only treatment in all but a handful of detention centers was to detox.
Some 630 of the roughly 5,000 jails and prisons nationwide now provide medication treatment for opioid use, according to the nonprofit Jail and Prison Opioid Project, up from about 20 in 2015. The drugs include buprenorphine, which tamps cravings for opioids, naloxone, which reverses their effects, and methadone, which eases withdrawal symptoms. Some are taken daily, others can be taken once a month in extended-release versions. The Biden administration said it wants medication available for every drug user in federal custody and at half of state prisons and jails by 2025.
