Based on the Centers for Disease Control’s (CDC) Covid Data Tracker and using Thursday as the first day of the week, here is the FEHBlog’s 2022 weekly chart of new Covid cases:
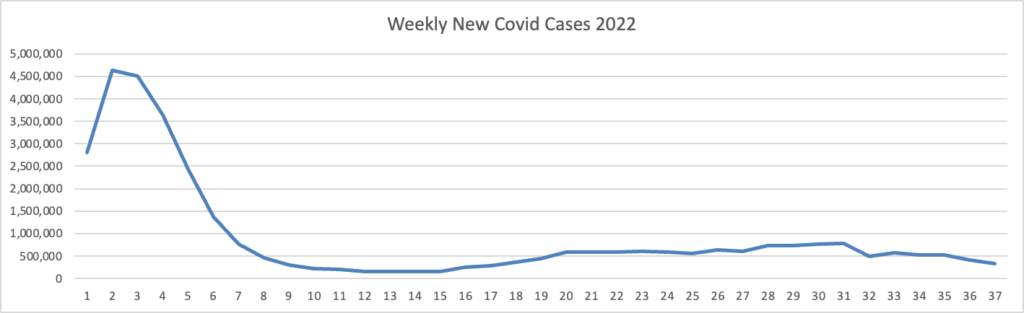
The bulge on the left is the first strain of Omicron.
The CDC’s weekly interpretative summary adds,
As of September 14, 2022, the current 7-day moving average of daily new cases (59,856) decreased 15.9% compared with the previous 7-day moving average (71,190).
CDC Nowcast projections* for the week ending September 17, 2022, estimate that the combined national proportion of lineages designated as Omicron will continue to be 100%. There are five lineages designated as Omicron: BA.5, BA.4.6, BA.4, BF.7, and BA.2.75. UPDATE: BF.7 has been separated from BA.5 and BA.2.75 sublineage is separated from BA.2 due to their positive growth rate. Until last week, these were aggregated with BA.5 and BA.2, respectively. The predominant Omicron lineage is BA.5, projected at 84.8% (95% PI 83.2-86.3%).
Here is the CDC’s chart of daily trends in new Covid hospitalizations:
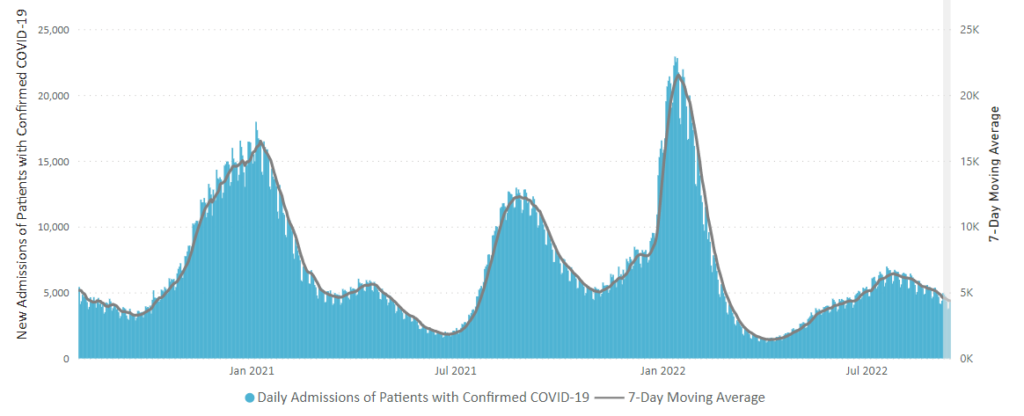
The CDC’s weekly interpretative summary adds “The current 7-day daily average for September 7–12, 2022, was 4,371. This is a 6.1% decrease from the prior 7-day average (4,657) from August 31–September 6, 2022.”
Here’s the FEHBlog 2022 weekly chart of new Covid deaths
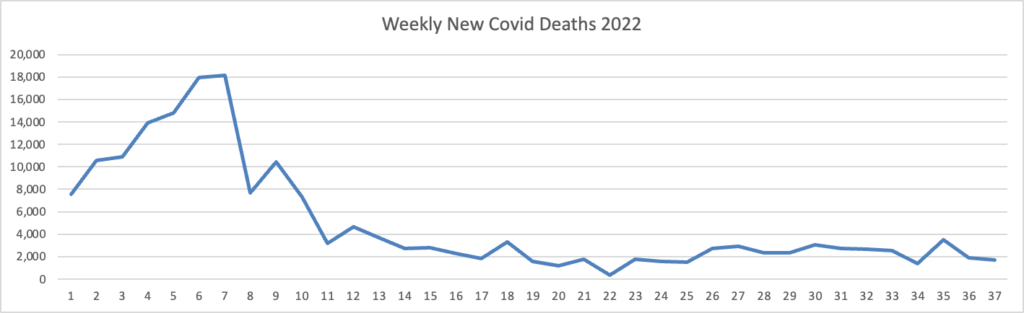
The CDC’s weekly interpretative summary adds, “The current 7-day moving average of new deaths (358) increased 3.9% compared with the previous 7-day moving average (344).”
The American Hospital Association points out that
In-hospital mortality among patients hospitalized primarily for COVID-19 fell from 15.1% during the delta period to 4.9% this April through June, the Centers for Disease Control and Prevention reported this week.
“In-hospital mortality risk was substantially lower during the later Omicron period overall and for older adults, persons with disabilities, and persons with multiple underlying medical conditions, who accounted for a larger proportion of hospitalizations in this period than they did during previous periods and remained at highest risk for death,” the authors said.
Here’s the FEHBlog’s chart of Covid vaccinations distributed and administered from the beginning of the Covid vaccination era in December 2020 through the 37th week of 2022. In the 37th week of this year, you will note a noticeable jump in distributions and administrations due to the release of bivalent mRNA booster.
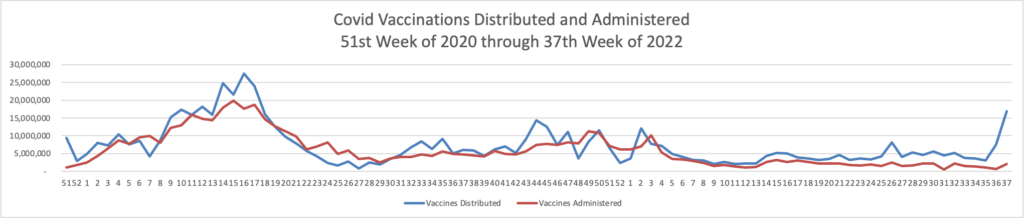
The CDC’s weekly interpretative summary adds,
As of September 14, 2022, 612.8 million vaccine doses have been administered in the United States. Overall, about 263.4 million people, or 79.3% of the total U.S. population, have received at least one dose of vaccine. About 224.6 million people, or 67.7% of the total U.S. population, have been fully vaccinated.
Of those fully vaccinated, about 109.2 million people have received a booster dose,* but 50.0% of the total booster-eligible population has not yet received a booster dose. Booster dose eligibility varies by age and health condition. Learn more about who is eligible.
The CDC’s Communities Levels experienced “Compared with last week, * * * a moderate decrease (−3.9 percentage points) in the number of high-level counties, a moderate decrease (-3.8 percentage points) in the number of medium-level counties, and a large increase (+7.4 percentage points) in the number of low-level counties.”
From the unusual viruses front —
- The AP reports that the CDC warns providers against giving the only monkeypox treatment Tpoxx “to otherwise healthy adults who are not suffering severe symptoms. ‘For most patients with healthy immune systems, supportive care and pain control may be enough,’ agency officials said in a statement.”
- The New York Times offers information on what parents should know about “the Latest Enterovirus Spike; The C.D.C. has issued an alert [to providers] about enterovirus D68, which has been linked to rare, polio-like paralysis.” In addition, the Times article advises soap and water handwashing and respiratory etiquette.
From the U.S. healthcare business front, we have two articles from Healthcare Dive.
- “Hospitals are likely to lose “billions of dollars” due to continued depressed margins and heightened labor costs, according to a report Thursday prepared for the American Hospital Association by Kaufman Hall. Even in the report’s optimistic model, more than half of all hospitals could end the year with negative margins, driven by an expected $135 billion increase in expenses this year and an $86 billion rise in labor costs alone.” Here’s a link to the article.
From the medical research front, we have two articles from STAT News:
- “CAR-T therapy isn’t exclusive to oncology: A half-dozen people with severe lupus, an autoimmune condition, have gone into remission after receiving an infusion of CAR-T cells, STAT’s Isabella Cueto reports. In lupus, B cells create antibodies against a person’s body, resulting in a vicious cycle of inflammation and immune attacks that lead to pain, fatigue, and organ damage. * * * Although the treatment has only been tested in six patients thus far, experts agree it is tantalizing.”
- “There hasn’t been much in the pharmaceutical arsenal to help people who abuse methamphetamines. But STAT’s Lev Facher reports that researchers are now studying a new monoclonal antibody, which binds to meth molecules and helps prevent them from entering the brain. The antibody is showing early promise in the smattering of emergency rooms involved in the study. One Phase 2 study is testing if the monoclonal antibody can treat meth overdose, and another is measuring its efficacy in helping long-term recovery. Ideally, the drug could be used for both purposes. The drug’s development is overseen by the University of Arkansas for Medical Sciences and the biotech InterveXion.”
From the miscellany front
- WTW released a study on how large employers are “doubling down on controlling healthcare costs and enhancing affordability.
- The National Committee for Quality Assurance released its Measurement Year 2021 health plan ratings.
- RevCycle Intelligence offers an interesting angle on a Health Affairs study of the efficacy of State No Surprise Billing laws in controlling out-of-network spending.
