From Capitol Hill, Roll Call reports
Third time’s a charm. Or so Democrats hope as they attempt to negotiate a third COVID-19 funding deal after their previous two bipartisan agreements — one for $15.6 billion in domestic and international aid, and a second for $10 billion in only domestic funds — stalled out.
The House is taking the lead on the latest iteration. But it’s not yet clear whether they’ll hold out for a bipartisan, bicameral agreement or attempt to move a Democrat-led version that would provide more funding, closer to President Joe Biden’s original $22.5 billion request.
“All the options are on the table,” House Majority Leader Steny H. Hoyer, D-Md., said Wednesday. “But it’s critical to get it done. And the fastest way to get it done is have an agreement on the four corners.”
From the No Surprises Act front, the U.S. Court of Appeals for the Fifth Circuit has granted the federal government/appellant’s “unopposed motion to stay further proceedings in this court pending ongoing rulemaking proceedings involving provisions of the No Surprises Act, with a status report due every sixty (60) days.” It’s worth noting that the final independent dispute resolution rule has not yet appeared on the OMB’s Office of Regulatory Affairs reginfo.gov site.
From the Omicron and siblings front, Fierce Healthcare tells us
Reported cases of COVID-19 and hospitalizations for the disease are on the rise across most of the U.S., with the Centers for Disease Control and Prevention (CDC) recently shifting many counties in the Northeast to medium or high levels of community risk. * * *
COVID-19 hospitalizations—which have become the CDC and other public health experts’ preferred metric for decisionmaking—have similarly begun to tick upward over the past month.
After reaching a seven-day average low of 1,426 daily admissions in early April, national admissions have continually increased and exceeded the seven-day average of 2,400 daily hospitalizations late last week. These new admissions represented an 11% increase over the previous week’s seven-day average, according to the agency, but were still nearly 90% below the January peak of more than 21,500 average daily admissions.
From the opioid epidemic front, the Wall Street Journal reports
Drug-overdose deaths in 2021 topped 100,000 for the first time in a calendar year, federal data showed, a record high fueled by the spread of illicit forms of fentanyl throughout the country.
More than 107,000 people in the U.S. died from drug overdoses last year, preliminary Centers for Disease Control and Prevention data released Wednesday showed, roughly a 15% increase from 2020. The proliferation of the potent synthetic opioid fentanyl has been compounded by the destabilizing effects of the Covid-19 pandemic on users and people in recovery, according to health authorities and treatment providers.
The U.S. has recorded more than one million overdose deaths since 2000, and more than half of those came in the past seven years.
“We’ve never seen anything like this,” said Robert Anderson, chief of the mortality-statistics branch at the CDC’s National Center for Health Statistics, regarding fentanyl’s impact on the numbers.
From the telehealth front, Healthcare Dive informs us
Telehealth visits for COVID-19 diagnoses fell in February, mirroring the sharp decline in new cases of the virus reported to the Centers for Disease Control and Prevention after January’s omicron-driven peak, according to Fair Health’s monthly telehealth claims tracker.
Overall telehealth use also slowed, falling 9.3% in February across the country. Virtual visits were 4.9% of all medical claim lines, down from 5.4% in the prior month.
With declining COVID-19 cases generating fewer telehealth sessions, mental health conditions accounted for a greater share of all diagnoses conducted via virtual platforms, according to the Fair Health data released Monday. Mental health diagnoses rose to about 64% of telehealth claims, up from 60% in January.
The FEHBlog is happy that people are using telehealth for mental healthcare,e which strikes the FEHBlog as a good, productive fit.
From the healthcare business front, Healthcare Dive reports
Advocate Aurora Health and Atrium Health said Wednesday they plan to merge, creating one of the nation’s largest nonprofit health systems with $27 billion in combined revenues and 67 hospitals across six states.
Board members from both systems unanimously approved the agreement, which is subject to regulatory review. The combined entity will be led by both CEOs for the first 18 months, at which time Advocate’s CEO Jim Skogsbergh will retire, leaving Atrium’s CEO Eugene Woods as sole leader.
Advocate and Atrium will have an equal number of board seats. Atrium’s board chair Edward Brown will first serve as chair until the end of 2023, followed by a two-year term for Advocate’s chair Michele Richardson.
The health systems’ joint press release adds
The new organization will have a combined footprint across Illinois, Wisconsin, North Carolina, South Carolina, Georgia and Alabama. It will serve 5.5 million patients, operate more than 1,000 sites of care and 67 hospitals, employ more than 7,600 physicians and nearly 150,000 teammates, and have combined annual revenues of more than $27 billion.
That’s an interesting combination.
Health Payer Intelligence calls attention to
Six technology vendors [who] were highlighted for their abilities to address one of the six main points of friction between payers and providers that leading healthcare organizations strive to address, according to a KLAS report that is part of the KLAS Payer/Provider Initiative.
KLAS launched the Payer/Provider Initiative to identify points of friction between payers and providers and to highlight strong collaboration case studies.
The six payer-provider challenges that leading healthcare organizations tackled were prior authorization, value-based care, payer-provider interoperability, denials, credentialing, and patient billing.
From the OPM front, Federal News Network tells us
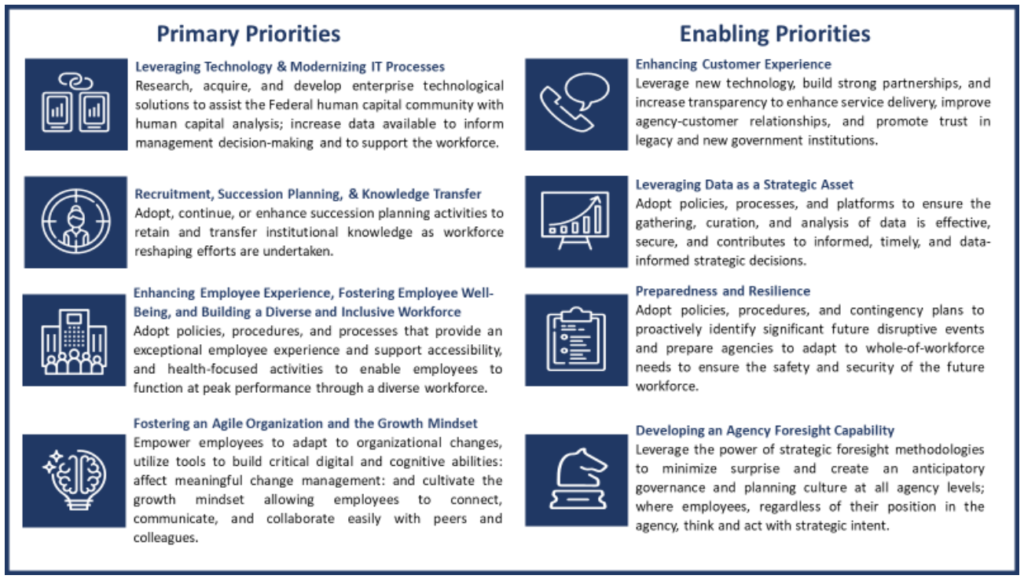
Agencies have to choose two out of four new focus areas to help improve their workforce over the next four years.
Deciding which options are most impactful gives agencies flexibility in how they approach new workforce objectives from the Office of Personnel Management.
Although OPM’s federal workforce priorities report, released on May 10, asks agencies to focus on only two of the four focus areas, implementing all four can help agencies resolve bigger workforce issues.
Among four primary priorities and four enabling priorities, OPM hopes agencies can implement proactive approaches to common issues, such as recruitment challenges.