
Congress is in session this week for committee business and floor voting. The big item is the omnibus spending bill which is expected to include the bipartisan COVID-19 relief package. The legislative language for this bill should be released tomorrow if everything remains on track. An omnibus or short term spending measure must be passed by 11:59 pm on December 11. The FEHBlog thought that both Houses of Congress were set to adjourn this week but it turns out that the Senate is scheduled to continue working through December 18.
The Federal Employee Benefits Open Season continues through next Monday December 14, while the Medicare Open Season ends tomorrow December 7. Let’s not forget that December 6 though 12 is the Centers for Disease Control’s (“CDC”) National Flu Vaccination Week.
The press is reporting tonight that President-elect Biden intends to appoint California Attorney General Xaxier Becerra to be his Secretary of Health and Human Services, which is a very powerful position when it comes to healthcare in the U.S. Speaking of healthcare leaders, Fierce Healthcare identifies six health plan executives to watch in 2021.
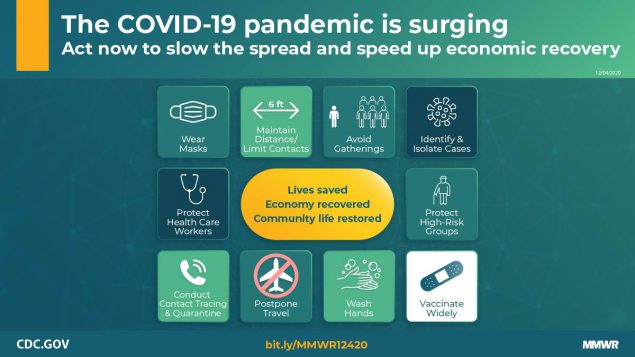
The CDC released updated COVID-19 protection guidance on Friday.
Summary
What is already known about this topic?The United States is experiencing high levels of SARS-CoV-2 transmission.
What is added by this report?
COVID-19 pandemic control requires a multipronged application of evidence-based strategies while improving health equity: universal face mask use, physical distancing, avoiding nonessential indoor spaces, increasing testing, prompt quarantine of exposed persons, safeguarding those at increased risk for severe illness or death, protecting essential workers, postponing travel, enhancing ventilation and hand hygiene, and achieving widespread COVID-19 vaccination coverage.
What are the implications for public health practice?
These combined strategies will protect health care, essential businesses, and schools, bridging to a future with high community coverage of effective vaccines and safe return to more activities in a range of settings.
The FEHBlog ran across a Bloomberg report which adds
Harvard disease expert Willam Hanage says that the science to date points to the primary risk coming from what he calls the three C’s — close contact, closed spaces and crowds. He says in Japan, where they’ve had few Covid-19 deaths, people are advised to avoid these — not just to wear masks in these situations but to limit them or avoid them altogether.

In much better but nevertheless thought provoking news, the Wall Street Journal reports that
Drug development for sickle-cell disease, largely overlooked for decades, is becoming a crowded field: Two papers published Saturday in the New England Journal of Medicine report promising results from studies of experimental therapies, including Crispr gene editing, for the disease.
In addition, Beam Therapeutics Inc. on Saturday presented lab and mouse data at the American Society of Hematology annual meeting to support the safety of another approach to using Crispr gene editing for sickle-cell disease. The company said it hopes to open a trial next year.
More than a dozen companies are competing to develop experimental treatments for sickle-cell disease, an inherited form of anemia that affects 100,000 mainly Black Americans.
The article points that Crispr gene editing is an expensive technology. “What good are new therapies for a disease if many patients suffering with it are unable, or choose not, to access them?” That is an issue for health plans to contemplate now, in the FEHBlog’s opinion.
The FEHBlog took a look at the CDC’s Center for National Health Statistics website today, and he ran across these interesting recent reports
- Increases in Prepregnancy Obesity: United States, 2016–2019 and
- Urgent Care Center and Retail Health Clinic Utilization Among Children: United States, 2019
The FEHBlog was surprised by the facts that “Prepregnancy obesity [measured as body mass index of 30 or higher] in the United States rose from 26.1% in 2016 to 29.0% in 2019 and increased steadily for non-Hispanic white, non-Hispanic black, and Hispanic women” and that “In 2019, more than one in four children had one or more visits to an urgent care center or retail health clinic (26.4%) in the past 12 months.” These reports further find that college educated women are less likely to be obese and that insured children are more likely to us retail health clinics.
The prepregnancy obesity report led the FEHBlog to consult OPM’s available statistics on federal employee demographics which date back to 2017. Roughly 52% of federal employees have at least college degree. The FEHBlog also found a May 2020 Pew Research report on Postal Service employee demographics which does discuss Postal employee education levels but does point out that
- About six-in-ten of the agency’s employees – including mail carriers, postal clerks, and mail sorters and processors – are non-Hispanic white (57%), compared with 78% of the overall U.S. workforce. Around a quarter (23%) of Postal Service workers are black, 11% are Hispanic and 7% are Asian. In contrast, black Americans make up 13% of the national workforce, Hispanics 17% and Asian Americans 6%.
- In 18 states and the District of Columbia, women make up half or more of Postal Service employees. In D.C., 74% of Postal Service workers are women, and women account for around six-in-ten postal workers in Idaho, Alabama and South Dakota. Nationally, slightly fewer than half of postal workers are women (45%), in line with the U.S. workforce.
- The Postal Service, as of 2018, employs more than 100,000 military veterans, who make up 16% of its workers nationally. Veterans account for just 5.8% of all employed Americans, according to data for 2019.
The percentage of women Postal employees basically aligns with the percentage of women federal employees. However, the percentage of military veteran Postal Service employees is nearly double the percentage of military veteran federal employees. (The FEHBlog also found this recent, helpful Congressional Research Service report on “Federal Workforce Statistics Sources: OPM and OMB.”)
The FEHBlog points this out because as the COVID-19 public health emergency has ably illustrated race, ethnicity, age and gender, among other demographic factors, impact healthcare and while OPM provides age and gender information to FEHB plans, the agency does not provide race or ethnicity date to those FEHB plans.
Finally the Salt Lake City [UT] Tribune reports that
More than a week after Sanford Health parted ways with its longtime CEO, the health system announced that it has indefinitely suspended merger talks with Utah-based Intermountain Healthcare. Sanford Health and Intermountain Healthcare made the announcement Friday [December 4], saying that with the leadership change, Sanford decided to put merger talks on hold while other organizational needs are addressed.
Intermountain offers an FEHB plan under the SelectHealth name.
